Quality improvement (QI) in healthcare isn't about pointing fingers when things go wrong. Instead, it’s a systematic, data-driven framework for looking at how we deliver patient care and asking one simple, powerful question: "How can we do this better?" It's a proactive mindset focused on making care safer, more effective, and more efficient by refining the very systems and processes we use every day, from patient check-in to post-discharge follow-up.
What is Quality Improvement in Healthcare, Really?

Think of it this way: a championship sports team doesn't just blame a player for a missed shot. They review the game tape to see what went wrong with the play itself. Was the pass off? Was the defensive setup weak? They look at the system, not just the individual.
That's exactly what quality improvement does in a clinical setting. It examines the entire patient journey—from the moment they try to book an appointment to their follow-up care after discharge—to spot the bottlenecks, communication breakdowns, and workflow snags that get in the way of excellent care. This approach is founded on the principle that most errors are not caused by bad people, but by flawed systems.
This represents a huge shift in perspective. It moves away from a culture of blame and empowers frontline healthcare workers—the real experts on the ground—to identify and fix the systemic issues they face daily. The core idea is that great people often work in flawed systems, and fixing the system is the surest path to better, more reliable patient outcomes and a safer work environment for clinicians.
Why Quality Improvement is a Global Priority
The push for better quality isn't just a "nice-to-have." It's a critical global health issue with life-or-death consequences. The World Health Organization (WHO) has some sobering statistics on this. In low- and middle-income countries, between 5.7 and 8.4 million deaths each year are directly attributable to poor-quality care.
That's up to 15% of all deaths in those regions. This stark data shows that simply having access to care isn't enough; the quality of that care is often the bigger, more life-threatening barrier. This makes a structured approach to improving healthcare delivery an absolute necessity for saving lives, reducing suffering, and building resilient health systems worldwide.
The Six Domains of Healthcare Quality
So, what does "good" quality actually look like? To give everyone a clear, common goal, the Institute of Medicine (now the National Academy of Medicine) outlined six key areas that high-quality healthcare must address. These domains act as a North Star for any QI initiative, providing a comprehensive framework for what excellence in healthcare truly means.
The central idea of quality improvement is to constantly ask, "How can we do this better?" It is a continuous journey of measurement, analysis, and refinement, driven by data and a commitment to patient well-being.
To truly understand what we're aiming for, let's break down these six pillars. They create a balanced framework for measuring and improving how care is delivered, ensuring that improvements in one area don't come at the expense of another.
The Six Domains of Healthcare Quality
| Quality Domain | Description |
|---|---|
| Safety | First and foremost, do no harm. This means protecting patients from injuries related to the care that's supposed to help them. This includes preventing errors, infections, and other preventable adverse events. |
| Effectiveness | Making sure care is grounded in science. It's about providing evidence-based services to those who will benefit and avoiding them for those who won't. This prevents both underuse and overuse of medical procedures. |
| Patient-Centeredness | Treating the person, not just the condition. This means respecting and responding to each patient's unique preferences, values, needs, and cultural background in all clinical decisions. |
| Timeliness | Reducing frustrating waits and harmful delays. This applies to patients needing care and the clinicians trying to provide it, ensuring prompt access to services to achieve the best possible outcomes. |
| Efficiency | Cutting out waste wherever it exists—whether it's wasted supplies, time, energy, or ideas. This includes optimizing workflows, reducing administrative burden, and ensuring cost-effective care. |
| Equity | Delivering high-quality care to everyone, regardless of their gender, ethnicity, geographic location, socioeconomic status, or other personal characteristics. This domain aims to close health disparity gaps. |
Making meaningful improvements across these areas often requires dedicated resources and funding. Organizations frequently turn to options like healthcare grants to support these vital projects. By keeping these six domains in focus, healthcare systems can build a more reliable, responsive, and compassionate experience for every single patient.
The Real-World Tools Driving Change
Knowing you want to improve quality is one thing. Knowing how to do it is another challenge entirely. This is where proven, structured methodologies come in. They provide the roadmaps that turn good intentions into organized, measurable action, ensuring that efforts are systematic rather than haphazard.
Instead of taking wild guesses or rolling out massive, risky changes, these frameworks help healthcare teams test ideas, see what the data says, and fine-tune their approach step by step. They are the practical tools that break down big, complex problems into manageable pieces, fostering a culture of continuous learning and improvement.
Let’s walk through three of the most trusted and widely used methodologies in healthcare today: PDSA, Lean, and Six Sigma. Each offers a different, yet powerful, way to look at and improve how things get done.
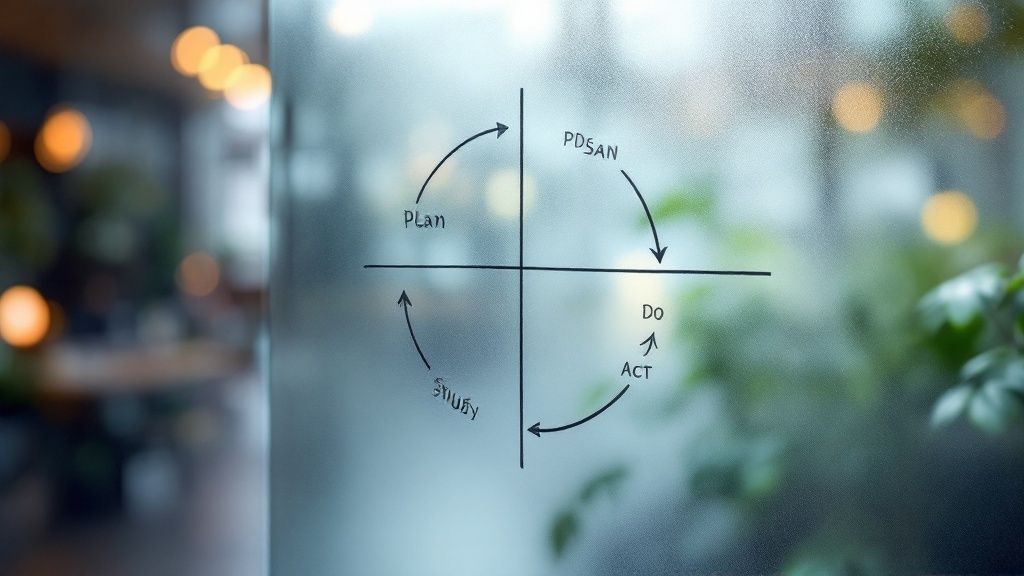
PDSA Cycle: The Scientific Method for Healthcare
The Plan-Do-Study-Act (PDSA) cycle is the absolute bedrock of quality improvement. The best way to think about it is as the scientific method, just adapted for a busy clinic or hospital floor. It’s all about making small, rapid tests of change, which lets teams learn quickly and adapt without bringing the whole system to a halt.
This cycle is beautifully simple but incredibly powerful. It breaks the whole improvement process into four common-sense steps:
- Plan: Your team spots a problem and comes up with a hunch—a hypothesis—for a small change that might make things better. You decide what to test, who's going to do it, how long the test will run, and what numbers you need to watch to see if it worked.
- Do: Now you run the test, but on a small scale. Maybe you try a new patient handoff script with just one nurse during a single shift, or implement a new checklist in one exam room for a day.
- Study: Time to look at the data you collected. Did the change actually work like you thought it would? Were there any surprises or unintended side effects? This phase is about objective analysis of both quantitative and qualitative feedback.
- Act: Based on what you learned, you decide on the next move. You might adopt the change as is, tweak it based on the results and run another PDSA cycle, or scrap the idea and try a different approach.
This constant looping prevents teams from pouring time and money into a big idea that ultimately fails. It builds confidence through small wins and makes sure every change is backed by real evidence from your own unique environment.
Lean: Eliminating Waste to Maximize Patient Value
Originally born in manufacturing with the Toyota Production System, Lean thinking has become a game-changer in healthcare. The core idea is brilliantly straightforward: find and get rid of any step in a process that doesn’t add value for the patient.
Picture a top chef running a world-class kitchen. Every movement is deliberate, every ingredient has a purpose, and absolutely nothing is wasted. Lean brings that same intense focus to healthcare workflows, whether it’s patient admissions, lab result turnaround, or operating room setup.
The goal is to streamline everything to be faster, more efficient, and totally centered on the patient. This means hunting down common types of "waste" you find in any clinical setting.
In the world of Lean, waste isn't just about tossing out unused supplies. It’s the time patients spend waiting for a doctor, the effort staff waste walking back and forth for equipment, and the untapped potential of skilled professionals stuck doing paperwork.
Common targets for Lean include:
- Waiting: Patients waiting for their appointment; staff waiting for lab results.
- Overproduction: Prepping meds or supplies long before they’re actually needed.
- Transportation: Needless movement of patients, samples, or equipment.
- Defects: Medical errors, billing mistakes, or infections that require costly rework.
- Inventory: Holding excess supplies that may expire or take up valuable space.
- Motion: Unnecessary movement by staff, like searching for equipment.
- Over-processing: Performing unnecessary tests or steps that don't add value.
By mapping out these processes and cutting out the wasteful steps, hospitals and clinics create a smoother, safer, and far more satisfying experience for everyone involved. You can dive deeper into how this works in our guide on healthcare process improvement.
Six Sigma: The Data-Driven Detective
If Lean is the efficiency expert focused on flow, then Six Sigma is the data-obsessed detective focused on stamping out critical errors and reducing variability. It’s a highly disciplined, statistical method for refining a process until mistakes become almost impossible.
The name "Six Sigma" actually comes from a statistical goal: achieving a process that produces no more than 3.4 defects per million opportunities. When you’re talking about surgery, giving medication, or processing lab samples, that level of near-perfection isn’t just a nice-to-have—it’s a necessity for patient safety.
Six Sigma projects usually follow a five-phase roadmap called DMAIC:
- Define: Pinpoint the exact problem, the project goals, and what success looks like from a patient and business perspective.
- Measure: Collect baseline data to get a clear, unbiased picture of how the process is performing right now. This establishes the starting point.
- Analyze: Dig into the data using statistical tools to find the true root causes of the defects. This step moves beyond symptoms to identify the core issues.
- Improve: Design, test, and implement solutions that directly address those root causes identified in the analysis phase.
- Control: Put monitoring systems and standard operating procedures in place to make sure the fix sticks and the problem doesn’t creep back in over time.
This rigorous, data-heavy approach is perfect for cracking tough cases where the cause isn't obvious, like reducing surgical site infections or figuring out why medication errors keep happening. By letting the data do the talking, Six Sigma helps teams solve the right problem with the right solution.
Measuring What Matters in Healthcare Quality

In healthcare, good intentions just don't cut it. There's an old business saying, "If you can't measure it, you can't improve it," and nowhere is that more true than when a patient's well-being is on the line. To make real progress, healthcare organizations have to look past vague goals and zero in on specific, measurable data points that show the real-world impact of their efforts.
These data points are called Key Performance Indicators (KPIs). Think of them as the vital signs for a healthcare system. Just like a doctor checks a patient's heart rate or blood pressure, an administrator tracks KPIs to gauge the health of their processes and confirm that improvement initiatives are actually making a difference.
Ultimately, these metrics are what turn the idea of quality improvement into a concrete, practical discipline. They offer clear, objective proof of what’s working, what isn’t, and where to direct your energy next.
The Three Pillars of Healthcare KPIs
To get the full picture of performance, healthcare KPIs are usually grouped into three main categories. Each one highlights a different—but equally critical—part of the patient's journey and the care system itself. Let's break down these pillars.
- Patient Safety: This is the bedrock. It’s all about upholding the first rule of medicine: do no harm. KPIs here track how often preventable mistakes and negative events occur.
- Clinical Effectiveness: This pillar measures how well treatments and care plans actually work. The goal is to ensure care is based on solid evidence and leads to the best possible health outcomes.
- Patient Experience: This category looks beyond clinical results to understand how patients feel about their care. It covers things like communication, compassion, and respect.
Looking at performance this way ensures that making things better in one area doesn't accidentally cause problems in another. For instance, a push for greater efficiency should never come at the cost of patient safety or satisfaction.
Key Metrics for Patient Safety
Patient safety is non-negotiable. Tracking these metrics is absolutely essential for spotting risks before they can cause serious harm.
One of the most important KPIs is the Hospital-Acquired Infection (HAI) Rate. This measures infections patients pick up while being treated for something else, like a bloodstream infection from a central line. A high rate is a major red flag, often pointing to issues with hygiene or sterilization.
Another crucial metric is the Medication Error Rate, which tracks mistakes in prescribing, filling, or giving medication. Driving this number down is always a top priority, as these errors can have devastating consequences.
Measuring Clinical Effectiveness
These KPIs give you a direct look at how well a healthcare organization is doing its most important job: helping people get better.
Hospital Readmission Rates are a classic example. This metric shows how many patients end up back in the hospital within 30 days of being sent home for the same issue. A high rate can signal that patients were discharged too early or didn't get the right education and follow-up care.
Another key measure is Adherence to Treatment Protocols. This tracks how consistently care teams follow established, evidence-based guidelines for specific conditions, like heart failure. High adherence means every patient is getting the standard of care that's been proven to work best. When tracking outcomes, the data has to be reliable. For example, understanding the accuracy of personal ECG devices shows just how much the precision of monitoring tools can affect the data used for quality improvement.
Gauging the Patient Experience
A good patient experience is closely tied to better health outcomes and patient loyalty, which is why leaders are paying more attention to it than ever. In fact, a recent Deloitte survey showed that 72% of healthcare C-suite executives see improving the consumer experience as a top priority.
Patient experience metrics are a direct reflection of how well a healthcare system respects patient dignity, preferences, and time. They measure the human side of care.
Common KPIs here include Average Patient Wait Times, from the moment someone checks in to when they see a provider. Long waits are a huge source of frustration and can signal underlying problems with scheduling or workflow.
Patient Satisfaction Scores, often gathered through surveys like HCAPS (Hospital Consumer Assessment of Healthcare Providers and Systems), give you direct feedback on everything from a doctor's communication style to the cleanliness of the waiting room. These scores help organizations find specific areas that need attention, from the front desk all the way to the operating room. To learn more about improving these workflows, check out our guide on electronic health record optimization.
The Real-World Benefits of Better Healthcare Systems

It’s one thing to talk about frameworks and metrics, but the real power of quality improvement comes alive when you see the difference it makes in people's lives. When a healthcare system truly commits to getting better, the positive effects are felt everywhere—by patients, by the medical staff, and across the entire organization.
We're not just talking about minor tweaks here. This is about building a safer, more effective, and more compassionate way to deliver care from the ground up.
A Better Experience for Patients
For anyone seeking care, the impact of quality improvement is deeply personal. It’s the difference between feeling lost in a confusing system and feeling genuinely supported and safe.
The most obvious win is a sharp drop in medical errors. Good QI work means fewer hospital-acquired infections, medication mix-ups, and wrong diagnoses. It creates an environment where people can heal without unnecessary risk.
This naturally leads to better health outcomes. When care follows proven best practices, patients recover faster, manage chronic diseases more effectively, and avoid preventable complications. But beyond the clinical charts, there’s a human side to it all. Smooth, patient-first processes mean shorter wait times, clearer communication, and a sense that you are being heard. That trust is everything.
Empowering Healthcare Professionals
Quality improvement isn't just another box to check on a busy clinician's to-do list; it’s a tool to make their jobs better. Anyone who has worked in a hospital knows the frustration of clunky workflows and constant workarounds—major drivers of burnout.
By focusing on fixing these broken processes, QI gives staff the power to solve the problems that make their days harder. The benefits are immediate:
- Less Administrative Hassle: Smarter charting and scheduling systems mean less time fighting with a computer and more time with patients.
- Higher Job Satisfaction: When you can do your job without constantly battling the system, morale naturally improves.
- A Culture of Ownership: QI invites frontline staff to identify issues and test solutions, giving them a real voice in how their workplace runs.
Quality improvement shifts the work environment from one of frustration to one of continuous learning. It directly tackles the root causes of staff burnout.
Focusing on smoother workflows is a huge part of achieving better hospital operational efficiency. At the end of the day, a happier, more engaged team provides better, more compassionate care. It's that simple.
Strengthening the Entire Healthcare System
When quality becomes the default setting, the entire system gets stronger, more cost-effective, and more trusted by the community it serves.
The financial upside is huge. By preventing medical errors, cutting out wasteful steps, and reducing costly readmissions, QI lowers the total cost of care. One study on antibiotic stewardship found that QI initiatives could cut the average number of IV antibiotic days by 10%, saving significant money while reducing patient risk.
That efficiency frees up resources that can be put back into innovation or community wellness programs. A system with a reputation for safety and quality earns public trust, which encourages people to be more proactive about their health. It creates a virtuous cycle: a healthier community and a stronger healthcare system, each supporting the other.
How Hospitals Improve Patient Care in Practice
Theory is one thing, but seeing quality improvement in action is where it really clicks. The true story of QI is found in the day-to-day work of clinical teams solving real problems.
Let’s look at a few examples of how these methodologies are applied in busy hospitals. Each case follows a familiar path: a team spots a recurring problem, picks the right tool for the job, and lets data guide them to a better way of doing things.
Case Study 1: Reducing Patient Falls with the PDSA Cycle
A general medical ward in a community hospital was seeing a disturbing rise in patient falls, especially among their older patients. These weren't just numbers on a chart; each fall meant potential harm, increased anxiety, and longer, more expensive hospital stays. The team decided to tackle this head-on using the quick and practical PDSA cycle.
-
Plan: The team had a hunch: inconsistent use of bedside safety checklists was a big part of the problem. They planned a small-scale test—a simplified, more visual checklist to be used by just two nursing shifts on one wing of the ward.
-
Do: For one week, the designated nurses used the new checklist at the start of every shift. They tracked every use and, crucially, every fall in their section, comparing their results to the rest of the ward.
-
Study: The data was crystal clear. The wing using the new checklist had zero falls. The other sections had three. Nurses also gave great feedback, saying the visual format was faster and a much better reminder.
-
Act: With a successful test under their belts, the team rolled out the new checklist ward-wide. After a quick training session, it became a standard part of their workflow, leading to a remarkable 45% reduction in patient falls over the next quarter.
This is a perfect example of starting small to win big. By testing a simple change, the team got the proof they needed to implement a broader, life-saving solution.
Case Study 2: Slashing Wait Times with Lean Principles
A busy outpatient clinic was drowning in long wait times. Patients were frustrated, often waiting over an hour past their appointment time, and the staff was completely overwhelmed. The clinic manager recognized this as a workflow problem—a classic case for Lean principles, which focus on cutting out waste.
The first step was to create a detailed process map, literally drawing out every single step a patient takes from the moment they walk in to the moment they leave. This simple exercise immediately highlighted several glaring sources of "waste":
- Excessive Transportation: Patients were being bounced between the waiting room, exam rooms, and a separate room just for taking vital signs.
- Waiting: A massive bottleneck formed as everyone waited for the one medical assistant to become available.
- Unnecessary Motion: Nurses were constantly walking back and forth to a central supply closet for basic items like gloves or bandages.
Seeing the problems laid out so clearly, the team got to work. They equipped each exam room with its own basic supplies, ending the constant trips to the closet. They also cross-trained front-desk staff to take vitals during check-in, which completely broke up the bottleneck.
The results were stunning. The average patient wait time plummeted from 70 minutes to just 15 minutes.
Case Study 3: Decreasing Medication Errors with Six Sigma
A large academic hospital was dealing with a tricky and dangerous problem: medication errors during IV antibiotic administration. While the overall error rate was low, the potential for severe patient harm was incredibly high. This kind of complex, high-stakes issue was the perfect fit for the rigorous, data-driven approach of Six Sigma.
A team of pharmacists, nurses, and IT specialists assembled and began their investigation using the DMAIC framework.
In high-risk areas like medication administration, even tiny variations in a process can have devastating consequences. Six Sigma gives you the statistical tools to find and eliminate the root causes of these dangerous defects.
First, they Defined the problem and Measured the current process, confirming an error rate that, while small, was unacceptable. During the Analyze phase, they dove deep into the data and found a critical pattern: most errors occurred when physicians decided to switch a patient from an IV to an oral antibiotic. The process was inconsistent.
For the Improve phase, the team built an evidence-based decision-support tool directly into the hospital's electronic health record (EHR). This tool prompted physicians with clear clinical criteria for making the switch. Finally, in the Control phase, they set up automated dashboards to monitor how well the new protocol was being followed.
The project was a huge success, leading to a 70% reduction in IV-to-oral transition errors. It also saved the hospital an estimated $200,000 annually by cutting down on unnecessary IV drug use.
To help you see how these different approaches stack up, here’s a quick comparison of when you might use each one.
Comparing QI Methodologies in Practice
This table breaks down the three primary QI methodologies we've discussed. Think of it as a guide to help you match the right tool to the right healthcare challenge.
| Methodology | Core Focus | Best Used For | Example Application |
|---|---|---|---|
| PDSA Cycle | Rapid, small-scale, iterative testing | Simple, localized problems where solutions can be tested quickly. | Trying out a new patient handoff script on a single unit for one week. |
| Lean | Eliminating waste and improving workflow efficiency | Complex processes with identifiable bottlenecks, delays, or redundant steps. | Redesigning the patient discharge process to reduce delays and confusion. |
| Six Sigma | Reducing variation and eliminating defects | High-risk, data-intensive problems where precision is critical. | Reducing surgical site infections by standardizing sterilization protocols. |
Each methodology has its strengths. The key is understanding the nature of your problem—is it a simple workflow tweak, a system-wide efficiency drag, or a high-stakes safety issue? Choosing the right framework from the start sets your team up for success.
The Future of Quality Improvement in Healthcare
The world of healthcare quality improvement is changing, and fast. While the core principles we've relied on for years—like PDSA cycles and Lean thinking—are still the bedrock of QI, a new wave of technology is pushing us forward. We're finally moving from a reactive mindset of fixing problems after they happen to a proactive one where we can prevent them altogether.
This isn't just a hypothetical shift; there's serious money behind it. The global market for healthcare quality management was valued at around USD 5.31 billion and is expected to nearly double to USD 10.47 billion by 2030. What’s driving this growth? Mostly, the widespread adoption of cloud-based platforms and the integration of artificial intelligence into how we manage quality. You can discover more insights about the healthcare quality management market and see just how big this trend is becoming.
The Rise of Predictive Analytics
Artificial intelligence (AI) and machine learning are leading this charge. Instead of waiting for a patient to be readmitted or for a safety incident to be reported, AI-powered systems can sift through mountains of data to flag at-risk patients before things go wrong.
Think about it this way: imagine a system that constantly monitors a patient's lab results, vitals, and clinical notes. It's trained to spot a very specific, subtle combination of factors that point to a high risk of developing sepsis. This system can alert the care team hours—or even days—before a human clinician might notice the pattern. That early warning gives them a crucial window to intervene and potentially save a life.
This is what it means to be proactive. It allows us to focus our resources where they're needed most, moving from damage control to genuine prevention.
Unifying Data for Deeper Insights
Of course, for any of this advanced analysis to work, you need good, clean, comprehensive data. That’s why the push for truly unified Electronic Health Records (EHRs) is so important. When a patient’s information is scattered across different, siloed systems, you can't see the full picture. It’s like trying to solve a puzzle with half the pieces missing.
A single, unified EHR creates the foundation for meaningful analysis. It gives quality improvement teams the ability to:
- Track a patient’s journey across every department and care setting.
- Spot hidden patterns in adverse events that would otherwise fly under the radar.
- Measure the real impact of a QI project with far greater accuracy.
This centralized data hub is what makes modern, data-driven quality improvement possible.
Expanding Access Through Telehealth
Technology isn't just making us smarter; it's also breaking down the physical barriers to care. Telehealth has become an incredible tool for reaching patients who live in rural or underserved areas, giving them access to specialists and follow-up appointments without forcing them to travel for hours.
Telehealth is more than just a video call. It’s a way to deliver consistent, high-quality care no matter where a patient lives. It ensures that care continues seamlessly long after someone leaves the hospital.
From a quality standpoint, telehealth is a game-changer for reducing hospital readmissions. It makes post-discharge follow-ups simple and reliable. It also helps patients with chronic conditions stay on track through more frequent check-ins, which lets us catch small problems before they become big ones. By making healthcare more accessible and continuous, these technologies are fundamentally improving both patient outcomes and the efficiency of the entire system.
Your Healthcare Quality Questions, Answered
Getting into the nitty-gritty of healthcare quality can bring up some questions. Let's break down a few of the most common ones with clear, practical answers to help you understand how improving patient care actually works.
Quality Improvement vs. Quality Assurance: What's the Difference?
It's easy to mix these two up, but they serve very different purposes.
Think of Quality Assurance (QA) as the safety net. It's a reactive process focused on catching errors after the fact to make sure minimum standards are met. It’s about compliance—like auditing patient charts to see if they were documented correctly. QA asks, "Did we do this right?"
Quality Improvement (QI), on the other hand, is proactive. It’s not about just meeting a standard; it's about continuously raising it. QI is a collaborative effort to redesign systems so that errors don’t happen in the first place. It asks a much bigger question: "How can we do this better next time?"
Who Is Actually Responsible for Quality Improvement in a Hospital?
The short answer? Everyone.
While most hospitals have a dedicated QI team to lead and organize initiatives, a real culture of quality can't live in just one department. It has to be a shared responsibility, woven into the daily work of every single staff member.
This means:
- Nurses and surgeons on the front lines who spot opportunities for safer procedures.
- Pharmacists who see ways to reduce medication errors.
- Administrators who can redesign inefficient workflows.
- Even the environmental services team, who are vital to preventing infections.
Often, the most brilliant and effective ideas come directly from the people doing the work day in and day out. They know the system's pain points better than anyone.
How Can a Small Clinic Get Started with Quality Improvement?
You don't need a huge team or a massive budget. The secret is to start small and let your successes build on each other.
The best way for a small practice to begin is by picking one specific, recurring problem and tackling it with a simple tool like the PDSA cycle. Small wins create the momentum for bigger change.
For instance, maybe you're getting consistent complaints about long wait times on the phone. Gather a small team and test one tiny change. What if you tried a new call-routing script for just one afternoon? Measure what happens, talk about what you learned, and then decide if the idea is worth keeping, tweaking, or ditching.
By taking over routine administrative work like patient scheduling and intake, Simbie AI gives your team back the time and energy needed for meaningful quality improvement projects. Stop letting paperwork get in the way of progress. See how Simbie can free up your staff to focus on what really matters—improving patient outcomes—at https://www.simbie.ai.

