In the complex world of healthcare, the patient chart is more than just a record; it's the cornerstone of quality care, a critical tool for communication, and the foundation of sound clinical decision-making. Mastering the art of clear, concise, and comprehensive documentation can often feel like a challenge, yet it is absolutely essential for both patient safety and the operational efficiency of any practice. Whether you're a seasoned clinician looking to refine your methods, a medical student preparing for board exams, or an administrator aiming to improve workflow, understanding the nuances of different charting formats is crucial. For those preparing to apply their charting skills in a high-stakes exam environment, this comprehensive USMLE Step 3 CCS Cases guide offers invaluable practice scenarios that reinforce these core documentation principles.
This in-depth guide is designed to be your go-to resource for practical, high-level documentation skills. We will break down eight essential patient chart examples, moving beyond simple templates to provide a deep strategic analysis and actionable takeaways for each one. You'll not only learn the structure of common formats like SOAP notes and the Problem-Oriented Medical Record (POMR) but also understand the 'why' behind them, equipping you with the knowledge to choose the most effective structure for any clinical encounter.
Furthermore, we will explore common pitfalls to avoid in medical charting, ensuring your notes are not only accurate and clinically useful but also legally sound and compliant. We'll also touch on how modern technological tools, such as sophisticated AI voice agents, are revolutionizing the process of data capture by seamlessly inserting structured, validated data directly into Electronic Medical Records (EMRs). By the end of this comprehensive article, you will have a clear, replicable framework for creating patient charts that enhance care, streamline your workflow, and ultimately support your practice's long-term success. Let's dive into the detailed examples that will elevate your charting from a routine administrative task to a powerful clinical strength.
1. SOAP Note (Subjective, Objective, Assessment, Plan)
The SOAP note is arguably the bedrock of modern clinical documentation and remains one of the most essential patient chart examples for any healthcare professional to master. Developed by Dr. Lawrence Weed in the 1960s as a core component of the Problem-Oriented Medical Record (POMR), its highly structured format organizes patient data into four distinct and logical sections. This intuitive flow ensures that every clinical encounter is documented comprehensively, supporting sound clinical reasoning, promoting clear communication among care team members, and ensuring continuity of care across different settings.

The structure is universally recognized and taught, making it invaluable in multidisciplinary environments where nurses, physicians, therapists, and specialists need to quickly and accurately understand a patient's current status and care plan. It is a foundational component taught in nearly every medical and nursing school and is deeply integrated into the architecture of leading EHR systems like Epic, Cerner, and Meditech.
Strategic Breakdown of the SOAP Framework
The true power of the SOAP note lies in its deliberate and logical separation of information, which guides the clinician through a systematic process, moving from the patient's reported symptoms to a definitive plan of action.
- S – Subjective: This section meticulously captures the patient's story, preferably in their own words. It includes the chief complaint (CC), the detailed history of present illness (HPI), a thorough review of systems (ROS), and all relevant past medical, family, and social history. In essence, it is everything the patient tells you, providing the crucial context for the clinical encounter.
- O – Objective: In this section, you document quantifiable, observable, and measurable data. This encompasses vital signs (blood pressure, heart rate, temperature, etc.), physical exam findings from a head-to-toe or focused assessment, laboratory results, and findings from imaging reports. This section must contain impartial, reproducible facts that are not subject to interpretation.
- A – Assessment: This is the critical synthesis of all the subjective and objective information gathered. It contains the primary diagnosis, as well as any differential diagnoses that are being considered. The assessment explains the clinician's professional judgment, interpreting the data to form a cohesive clinical picture of the patient's condition.
- P – Plan: This final section outlines the comprehensive course of action for the patient. It details any medications to be prescribed, further diagnostic tests to be ordered, referrals to specialists, and specific patient education provided. Crucially, each part of the plan should directly address an issue identified in the assessment, creating a clear and justifiable care pathway.
Actionable Takeaways for Effective SOAP Charting
To create high-quality, defensible SOAP notes that enhance patient care, streamline billing, and mitigate risk, focus on precision, clarity, and logical consistency.
- Maintain Strict Boundaries: Scrupulously avoid mixing subjective statements with objective findings. For instance, the statement "Patient reports experiencing significant shortness of breath" belongs squarely in the Subjective section, while the finding "Respirations are 22/min with audible expiratory wheezing on auscultation" belongs in the Objective section.
- Be Specific and Measurable: Use precise clinical terminology and quantifiable metrics in the Objective section. Instead of a vague note like "high blood pressure," document the exact measurement: "BP 145/92 mmHg, right arm, seated." This level of detail is non-negotiable for accurate tracking and treatment.
- Link Plan to Assessment: Ensure every single element of your Plan directly corresponds to a diagnosis or problem listed in the Assessment. For example, if "Hypertension" is listed as problem #1 in the Assessment, the Plan should have a corresponding #1 that outlines the specific treatment for it. This creates a clear, defensible record of your clinical decision-making.
For those looking to deepen their understanding of documentation and explore how this fundamental format compares to other specialized structures, you can learn more about various medical report formats on Simbie.ai.
2. POMR (Problem-Oriented Medical Record)
The Problem-Oriented Medical Record (POMR) is a revolutionary and highly structured framework that organizes all patient information around specific, defined medical problems. Pioneered by Dr. Lawrence Weed in the 1960s, this sophisticated system represents a significant departure from traditional chronological or source-based record-keeping. Instead, it creates a dynamic and logical chart centered on a master "problem list," which serves as the central index for all clinical data. The POMR is one of the most influential patient chart examples because it forces a structured, disciplined approach to clinical reasoning and is exceptionally well-suited for long-term care management.
This method is particularly powerful and widely adopted in academic medical centers, tertiary care facilities, and any setting that manages patients with complex, chronic, and multifactorial conditions. By meticulously structuring all data, plans, and notes around numbered problems, it provides any member of the care team with an immediate, holistic, and easily navigable view of the patient's complete health status and the explicit rationale behind each clinical intervention.
Strategic Breakdown of the POMR Framework
The POMR's undeniable strength comes from its four interconnected components, which work in concert to create a comprehensive, organized, and easily auditable patient record. This structure promotes an unparalleled level of continuity of care, especially for patients with multiple comorbidities being seen by various specialists.
- Database: This serves as the foundation of the record, containing all initial patient information. It includes the chief complaint, a detailed history of the present illness, comprehensive past medical history, family history, social history, a full review of systems, and the findings from the initial physical examination.
- Problem List: This is the heart and soul of the POMR. It functions as a numbered, high-level index of every significant issue the patient has, including both active and resolved problems. A "problem" can be a formal diagnosis (e.g., Type 2 Diabetes), a specific symptom (e.g., Chronic Dizziness), a significant lab abnormality (e.g., Persistent Hyponatremia), or even a social issue impacting health (e.g., Homelessness).
- Initial Plans: For each individual problem identified and numbered on the list, a detailed initial plan is created. This plan is often structured using the familiar SOAP format and meticulously outlines the strategy for diagnostics, therapeutics, and patient education that is specific to that particular problem.
- Progress Notes: All subsequent entries into the patient's chart, including follow-up visits, new findings, and updates, are documented as progress notes. Critically, each note is explicitly titled and numbered to correspond directly with a specific problem on the master list, ensuring that every update is clearly contextualized and linked to a particular clinical issue.
Actionable Takeaways for Effective POMR Charting
To effectively leverage the POMR for superior patient management and enhanced clinical reasoning, a focus on meticulous organization, consistency, and regular updates is non-negotiable.
- Maintain a Dynamic Problem List: The problem list is not a static document. It must be actively reviewed, updated, and reconciled at every single patient encounter to accurately reflect new diagnoses, resolved issues, and any changes in the status of existing problems.
- Number and Title Everything Consistently: Rigorously number and title each problem on the master list. Then, use that exact same number and title for every progress note, medical order, and care plan element related to it. This creates an unambiguous and easily followed trail of logic for anyone reviewing the chart.
- Explicitly Link Plans to Problems: Every single order, prescription, referral, or intervention must be explicitly linked back to a numbered problem on the list. This ensures that the clinical reasoning behind every action is transparent, defensible, and clear, which is absolutely critical for complex care coordination and patient safety.
The POMR remains a gold standard for teaching structured clinical reasoning and is a foundational concept that has heavily influenced the design of many modern EHRs. For more on organizational frameworks, you can explore the principles of structured clinical documentation on the Agency for Healthcare Research and Quality (AHRQ) website.
3. HPI (History of Present Illness) Template
The History of Present Illness (HPI) is the narrative heart of any patient encounter, and utilizing a structured template is a critical skill demonstrated in the very best patient chart examples. This methodological approach transforms a patient's story from a simple anecdote into a diagnostically powerful report by methodically exploring every facet of their chief complaint. It systematically organizes the intricate details of a symptom's journey—from its initial onset to the present moment—providing the rich clinical context needed for an accurate differential diagnosis and the development of an effective treatment plan.
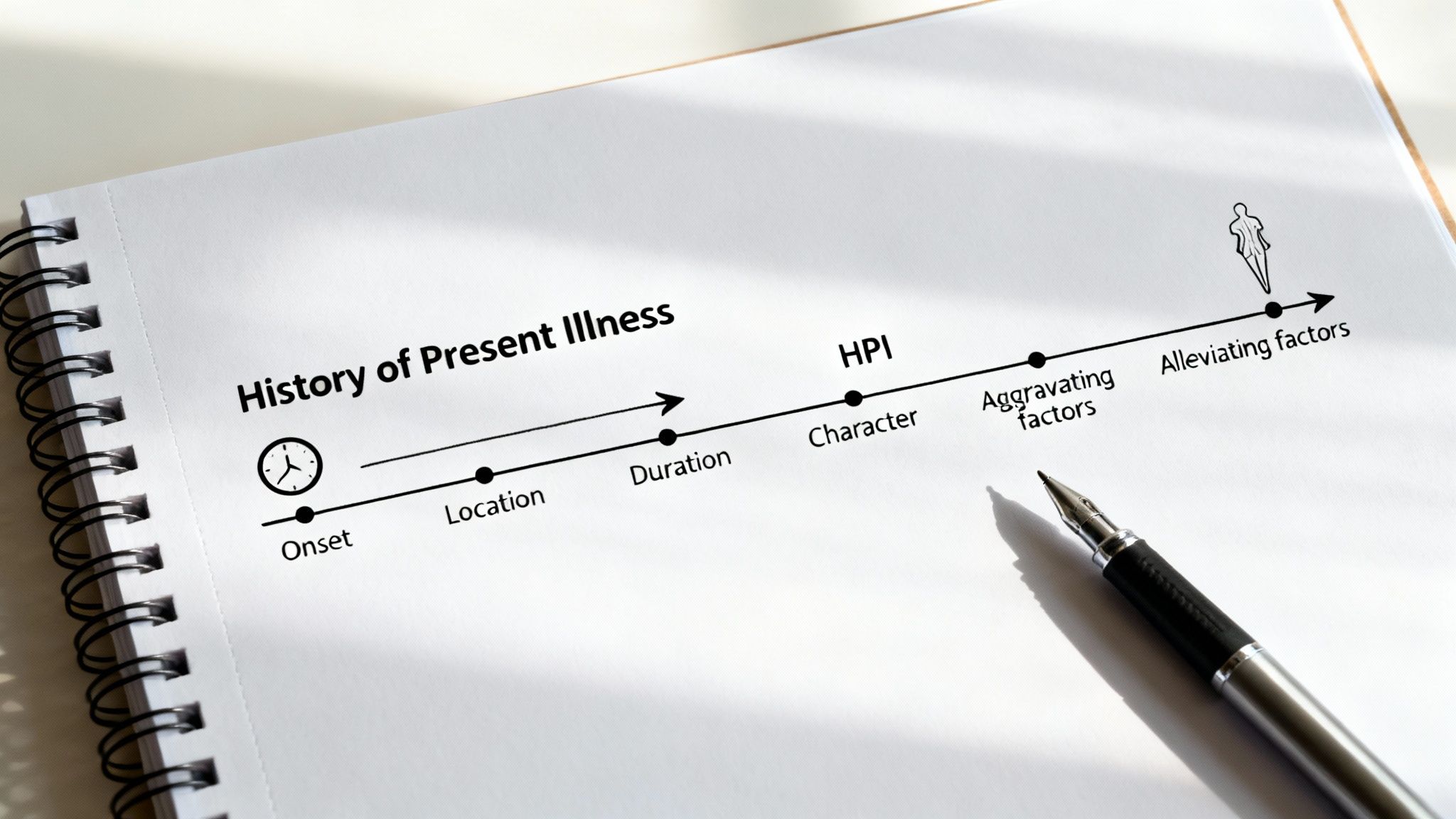
Popularized throughout medical training and deeply embedded within the workflows of modern EHRs, the HPI template ensures that no critical detail is overlooked during the information-gathering process. Its systematic, almost investigative, approach is invaluable in high-pressure settings like emergency departments, urgent care clinics, and initial specialist consultations, where distinguishing between similar presentations quickly and accurately is absolutely essential for patient safety.
Strategic Breakdown of the HPI Framework
The undeniable strength of a well-structured HPI lies in its investigative framework, often guided by widely-used mnemonics like OLDCARTS (Onset, Location, Duration, Character, Alleviating/Aggravating factors, Radiation, Timing, Severity). This framework guarantees a comprehensive and multidimensional evaluation of the patient's chief complaint.
- O – Onset: When exactly did the symptom begin, and under what circumstances? Was the onset sudden and dramatic, or was it gradual and insidious?
- L – Location: Where precisely is the symptom located? Is it localized to a specific point, or is it diffuse and widespread?
- D – Duration: How long has the symptom been present? Is it a constant sensation, or does it occur intermittently? If intermittent, how long do episodes last?
- C – Character: What does the symptom feel like to the patient? Encourage descriptive language (e.g., sharp, dull, aching, burning, pressure-like).
- A – Alleviating/Aggravating Factors: What actions, positions, or treatments make the symptom better or worse? This includes any over-the-counter or home remedies the patient has already tried.
- R – Radiation: Does the symptom travel or radiate to other parts of the body? For example, does the chest pain radiate to the left arm or jaw?
- T – Timing: Is there a discernible pattern to when the symptom occurs? (e.g., only in the morning, consistently after meals, during physical exertion).
- S – Severity: How severe is the symptom, typically rated on a standardized scale of 1 to 10? How does it compare to previous experiences of pain or discomfort?
Actionable Takeaways for Effective HPI Charting
To create a powerful HPI that actively drives clinical reasoning and leads to a more accurate diagnosis, focus on fostering narrative clarity while maintaining systematic inquiry.
- Start Broad, Then Narrow Down: Begin the conversation with a classic open-ended question like, "Tell me more about what brought you in today." Allow the patient to provide their initial story uninterrupted. Once they have, use the OLDCARTS framework to ask specific, targeted questions to meticulously fill in any missing details.
- Document as a Chronological Narrative: Structure the final HPI documentation as a clear, easy-to-follow timeline. Describe the logical evolution of the symptoms from when they first started to the present moment, including any notable changes in character, severity, frequency, or response to treatments.
- Include the Functional Impact: A crucial but often-missed element is documenting how the illness affects the patient's daily life and functional status. Note any impact on their ability to work, sleep, eat, or engage in routine activities. This provides a more complete clinical picture and helps in assessing the true severity of the condition.
Mastering HPI documentation is a fundamental skill for any practitioner. For tips on how to build efficient, customized HPI templates into your clinical workflow, you can find valuable strategies for Electronic Health Record optimization on Simbie.ai.
4. Chief Complaint (CC) and Review of Systems (ROS) Template
The Chief Complaint (CC) and Review of Systems (ROS) template serves as a foundational duo in clinical documentation, acting as the structured starting point for nearly every patient encounter. This powerful combination provides a framework that is both structured for consistency and patient-centered for relevance, making it one of the most vital patient chart examples for gathering comprehensive health information efficiently. The CC precisely captures the patient’s primary concern, ideally in their own words, while the ROS performs a methodical, head-to-toe symptom check across all major body systems.

This structured approach, which is taught universally in medical and nursing training and is embedded as a core feature in all major EHR systems, ensures that clinicians effectively address the immediate issue while also systematically screening for potential related or co-existing conditions that the patient might not have mentioned. Together, they form the core of the "Subjective" section in a standard SOAP note and are absolutely crucial for new patient evaluations, annual physicals, and complex specialist consultations.
Strategic Breakdown of the CC and ROS Framework
The power of this template lies in its effective two-part structure, which intelligently funnels the inquiry process from a very specific problem down to a broad, comprehensive health overview, thereby guiding a thorough and meticulous diagnostic process.
- CC – Chief Complaint: This is the patient's primary reason for seeking the medical visit, documented verbatim whenever possible to preserve its authenticity (e.g., "I've had a crushing pain in my chest for the last two hours"). The CC sets the immediate focus for the history of present illness (HPI) and guides the subsequent physical examination.
- ROS – Review of Systems: This is a systematic inventory of common symptoms across various organ systems, such as constitutional (fever, weight loss), cardiovascular (chest pain, palpitations), respiratory (cough, shortness of breath), and gastrointestinal (nausea, abdominal pain). It is typically performed using a checklist or a structured question-based format to quickly identify both positive and negative findings, which helps to rule in or rule out items on the differential diagnosis list.
Actionable Takeaways for Effective CC and ROS Charting
To create a clear, clinically valuable, and legally sound record using this template, clinicians should prioritize precision, context, and thoroughness.
- Quote the Patient Directly for the CC: For the Chief Complaint, always use the patient's exact words and place them in quotation marks. This practice preserves the raw, unfiltered nature of their primary concern and importantly avoids any premature clinical interpretation or bias on the part of the clinician.
- Tailor the Depth of the ROS: Skillfully adjust the scope and depth of the Review of Systems based on the specific clinical context. A focused ROS is often sufficient for a straightforward, isolated problem like an ankle sprain. In contrast, a comprehensive 14-point ROS is necessary for a new patient evaluation, an annual physical, or a complex diagnostic challenge to ensure no significant symptoms are missed.
- Diligently Document Pertinent Negatives: In the ROS, explicitly documenting the absence of key symptoms (known as pertinent negatives) is just as clinically important as noting positive findings. For a patient presenting with a cough, stating "Patient denies fever, chills, night sweats, and shortness of breath" provides critical diagnostic information that helps narrow down the potential causes.
5. Physical Examination (PE) Template
The Physical Examination (PE) template is an absolute cornerstone of clinical documentation, providing a highly structured framework for recording the objective findings from a patient's physical assessment. This essential tool ranks as one of the most fundamental patient chart examples, meticulously guiding clinicians through a systematic head-to-toe or system-by-system evaluation. Its standardized format not only ensures thoroughness and prevents critical omissions but also creates a clear, objective baseline that is indispensable for diagnosis, treatment planning, and monitoring patient progress over time.
Popularized through foundational clinical texts like Bates' Guide to Physical Examination and reinforced in medical training programs worldwide, the PE template is a critical component of new patient visits, hospital admissions, pre-operative clearances, and any comprehensive health evaluation. It serves the vital function of translating direct clinical observation, palpation, and auscultation into a permanent, shareable, and legally sound record within the Electronic Medical Record (EMR).
Strategic Breakdown of the PE Framework
The significant strength of the PE template lies in its organized, hierarchical structure. This design allows for both comprehensive, broad overviews required for annual physicals and focused, problem-oriented assessments tailored to a patient's specific complaint.
- General Appearance & Vital Signs: This initial section provides a crucial snapshot of the patient's overall health status at that moment. It includes core vital signs (Blood Pressure, Heart Rate, Respiratory Rate, Temperature, Oxygen Saturation), and a concise general statement on their appearance (e.g., "Patient is a well-developed, well-nourished male, alert and oriented, in no acute distress").
- System-Based Organization: Findings are methodically grouped by anatomical or physiological system (e.g., HEENT, Cardiovascular, Pulmonary, Abdominal, Neurological, Musculoskeletal). This logical flow ensures a systematic examination and makes it incredibly easy for other providers to locate specific information quickly when reviewing the chart.
- Detailed Findings within Each System: Within each system, the template prompts for the detailed documentation of specific observations gathered through the four main examination techniques: inspection, palpation, percussion, and auscultation. This is where precise clinical descriptions are recorded, forming the evidentiary basis for the assessment.
Actionable Takeaways for Effective PE Charting
To create high-quality, defensible PE notes that support an accurate diagnosis and facilitate clear team communication, focus on systematic documentation, objectivity, and precision in your language.
- Diligently Document Pertinent Negatives: Stating what is not found during the exam is equally as important as documenting positive, abnormal findings. For a patient presenting with a cough, noting "Lungs are clear to auscultation bilaterally, with no wheezes, rales, or rhonchi" is a critical piece of information that helps to narrow the differential diagnosis significantly.
- Be Specific, Objective, and Quantitative: Avoid vague, subjective terms. Instead of writing "abdomen seems okay," use precise clinical language: "Abdomen is soft, non-tender, and non-distended with normoactive bowel sounds in all four quadrants. No hepatosplenomegaly noted." Use measurements whenever possible (e.g., "Liver edge palpated 2 cm below the right costal margin").
- Tailor the Exam to the Presenting Complaint: While a complete head-to-toe examination is necessary for new patients or comprehensive physicals, subsequent or problem-focused visits require a tailored exam. If a patient presents with ankle pain after an injury, the PE should prioritize a detailed examination of the musculoskeletal and neurovascular systems of the affected lower extremity, along with any other relevant associated systems.
6. Problem List Template
The Problem List is a vital, at-a-glance summary of a patient's overall health status and stands as one of the most functional and high-impact patient chart examples within a modern Electronic Health Record (EHR). It is a dynamic, organized, and longitudinal compilation of all significant active and past medical, surgical, psychological, and social issues. Maintained over the course of a patient's entire care journey, this list provides any clinician with immediate, critical context, ensuring that chronic conditions and significant historical health events inform every single care decision made at the point of care.
This template is far more than just a passive medical history; it is a foundational, active tool for enhancing patient safety and coordinating care. It directly supports critical clinical tasks such as medication reconciliation, generating alerts for potential drug-disease contraindications, and justifying specialist referrals. Recognizing its importance, leading EHRs like Epic and Cerner feature the Problem List prominently on the patient's main dashboard or summary screen, underscoring its central role in modern clinical workflows.
Strategic Breakdown of the Problem List Framework
The unparalleled effectiveness of the Problem List comes from its meticulously organized and prioritized structure, which allows providers to quickly and accurately assess a patient's cumulative health burden and key risk factors.
- Active Problems: This is the most crucial and frequently referenced section, listing all current, ongoing conditions that require active management. This includes chronic diseases like Hypertension, Type 2 Diabetes, or Chronic Kidney Disease, as well as acute issues like a recent Myocardial Infarction or an active infection. Each problem is typically linked to a specific date of onset and a corresponding ICD-10 code for billing and data analysis.
- Historical/Resolved Problems: This section serves as an archive, documenting significant past issues that are no longer active but may have long-term implications or relevance for the patient's future health. Examples include a history of a major surgery (e.g., Cholecystectomy), a resolved cancer diagnosis (e.g., Breast Cancer in remission), or a past significant injury (e.g., Femur fracture).
- Social/Behavioral Problems: A modern and critically important addition to many problem lists, this area captures key social determinants of health (SDOH) that significantly impact medical outcomes. Items such as homelessness, food insecurity, lack of transportation, or tobacco use are documented here to provide a truly holistic and contextualized view of the patient's life and health challenges.
- Family History: While sometimes maintained as a separate section in the chart, significant hereditary conditions (e.g., family history of early-onset coronary artery disease or specific cancers) are often included directly on the problem list to keep genetic predispositions top of mind during routine diagnosis and preventative care planning.
Actionable Takeaways for Effective Problem List Management
To maintain an accurate, reliable, and clinically useful Problem List that genuinely enhances clinical decision-making and patient safety, diligence, standardization, and regular maintenance are absolutely key.
- Update at Every Single Encounter: Make it a non-negotiable standard practice to review and reconcile the problem list directly with the patient during every single visit. This ensures the list remains a "living document" that accurately and completely reflects their current health status and priorities.
- Use Standardized Terminology and Codes: Always link problems to standardized clinical terminologies like SNOMED CT and assign the most specific and appropriate ICD-10 code. This practice is crucial for supporting accurate billing, enabling population health analytics, facilitating clinical research, and ensuring interoperability between systems.
- Prioritize, Prune, and Organize: Regularly organize the list to highlight the most clinically significant and active problems at the top. Diligently move resolved issues to the historical list to keep the "Active Problems" section clean, focused, and relevant to immediate care needs. This critical step prevents cognitive overload for clinicians and reduces the risk of overlooking key issues.
7. Clinical Progress Note Template
The Clinical Progress Note is the narrative engine that drives ongoing patient care, serving to document the clinical course over time during a hospitalization or throughout outpatient treatment for a specific condition. It stands as a vital patient chart example for meticulously tracking a patient's journey, detailing subtle or significant changes in symptoms, documenting their response to specific interventions, and outlining any adjustments made to the overarching care plan. This chronological, episode-based record is absolutely essential for maintaining continuity of care and justifying the need for continued treatment or services.
These notes are a fundamental practice in both inpatient and outpatient settings, from the daily rounding notes in a hospital to the routine follow-up visit notes in a primary care clinic. Their primary purpose is to clearly and concisely communicate the patient's trajectory to the entire care team—including physicians, nurses, therapists, and consultants—ensuring everyone is aligned on the patient's current status, recent progress, and immediate next steps. They are often structured using established formats like SOAP (Subjective, Objective, Assessment, Plan) or APIE (Assessment, Plan, Intervention, Evaluation), making them a cornerstone of modern medical records.
Strategic Breakdown of the Progress Note Framework
A strong, effective progress note tells a concise and compelling story of change over a defined period. It builds upon the information from the previous entry to create a clear, logical, and easy-to-follow clinical timeline.
- Comparative Opening: The note frequently and effectively begins with a brief, direct comparison to the patient's previously documented state. For example, a note might start with, "Patient reports significantly improved pain control and increased mobility since yesterday's physical therapy session and medication adjustment."
- Focused Update on Changes: A well-written progress note documents only new or changed findings, deliberately avoiding the redundant repetition of information from previous notes. This disciplined approach keeps the patient record clean, concise, and easy for a busy clinician to review quickly.
- Intervention and Specific Response: This section details any treatments, therapies, or other interventions administered since the last note and, crucially, documents the patient's specific response to them. For example, "Administered 4mg IV morphine with good effect; patient reported pain decreased from 8/10 to 3/10 within 20 minutes."
- Revised Assessment and Adjusted Plan: Based on the updated subjective and objective information, the assessment of the patient's condition is refined, and the plan is modified to reflect their current needs, progress toward care goals, and any new issues that have arisen.
Actionable Takeaways for Effective Progress Notes
To write progress notes that are both efficient for the author and effective for the reader, prioritize clarity, conciseness, and unwavering relevance to the patient's clinical course.
- Start with the Status Change: Immediately orient the reader by stating how the patient is doing compared to the last assessment. Is their condition better, worse, or unchanged? This simple opening sets the context for the rest of the note.
- Vigorously Avoid Note Bloat: Resist the powerful temptation to simply copy and paste large sections of text from previous entries (a practice known as "copy-forward"). Each note should be a unique, time-stamped assessment that reflects the patient's current status and your clinical thinking for that specific encounter.
- Clearly Link Findings to Plan Changes: Explicitly connect your observations to your actions to demonstrate clear clinical reasoning. For instance, write, "Given the patient's persistent hypertension despite lisinopril 20mg daily, the plan is to add a low-dose diuretic, HCTZ 12.5mg daily." This shows a logical progression of thought and action.
Mastering this form of concise, targeted documentation is a key part of any successful clinical documentation improvement program that aims to enhance care quality, improve billing accuracy, and increase operational efficiency.
8. Assessment and Plan (A&P) Template
The Assessment and Plan (A&P) section is the critical synthesis component of a clinical note, where the clinician’s diagnostic reasoning and intended course of action are clearly and definitively documented. As a core component of many foundational patient chart examples, most notably the SOAP note, this section translates all the preceding subjective and objective data into a clear diagnosis (the Assessment) and a concrete, actionable care strategy (the Plan). It is the part of the patient chart that most clearly and powerfully demonstrates the clinician's medical judgment and decision-making process.
This template is fundamental across all medical specialties and practice settings, from managing a new diagnosis in a primary care office to handling an acute exacerbation of a chronic illness in the emergency department. The clarity and precision of the A&P are absolutely essential for effective care coordination, ensuring that every member of the healthcare team—from nurses to specialists to the patient themselves—understands the identified problems and the corresponding treatment goals.
Strategic Breakdown of the A&P Framework
The A&P's primary strength lies in its direct and explicit linkage between diagnosis and action. It masterfully bridges the gap between raw data collection and patient-centered treatment, creating a logical, transparent, and legally defensible record of clinical decision-making.
- A – Assessment: This is the clinician's professional summary and interpretation of the patient's condition. It includes the primary diagnosis and any relevant differential diagnoses, often presented as a numbered problem list for maximum clarity. Each assessment point should be directly supported by evidence from the subjective and objective sections of the note, effectively explaining the "why" behind each diagnosis.
- P – Plan: This section meticulously details the management strategy for each problem identified in the assessment. The plan must be specific, comprehensive, and unambiguous. It should cover all relevant domains: diagnostics (labs, imaging to be ordered), therapeutics (medications with dose and frequency, procedures), patient education (counseling provided, handouts given), referrals to specialists, and clear, time-bound instructions for follow-up.
Actionable Takeaways for Effective A&P Charting
To craft an A&P section that is exceptionally clear, clinically effective, and supportive of high-quality care, a focus on organization, specificity, and justification is paramount.
- Link Plan to Assessment Numerically: For optimal clarity and to eliminate any ambiguity, structure the A&P as a numbered problem list. The plan for problem #1 should directly and exclusively address the diagnosis listed as assessment #1. This format makes it incredibly easy for other providers, auditors, and even yourself to follow your thought process at a later date.
- Make All Plans Specific and Measurable: Vigorously avoid vague or imprecise instructions. Instead of writing "start blood pressure medication," document "Start Lisinopril 10 mg PO daily." Instead of the ambiguous "follow up as needed," specify "Follow up in my office in 2 weeks for a blood pressure recheck and to review today's lab results."
- Briefly Justify Your Reasoning: In the assessment portion, briefly include your clinical reasoning, especially for complex cases, new diagnoses, or situations with diagnostic uncertainty. For example, "1. Community-Acquired Pneumonia, diagnosis based on patient's presentation of fever, productive cough, and right lower lobe consolidation noted on chest X-ray." This adds significant clinical value and defensibility to your note.
8-Template Patient Chart Comparison
| Template | Implementation complexity 🔄 | Resource / Speed ⚡ | Expected outcomes 📊 | Ideal use cases 💡 | Key advantages ⭐ |
|---|---|---|---|---|---|
| SOAP Note (Subjective, Objective, Assessment, Plan) | Moderate — four-part structured workflow 🔄 | Efficient with EHR templates; moderate time upfront ⚡ | High documentation quality and continuity; medico-legal support 📊 | Routine outpatient visits, inpatient rounds, many specialties 💡 | Standardized, easy to navigate; improves clinical reasoning ⭐ |
| POMR (Problem-Oriented Medical Record) | High — problem-centric setup and linkage required 🔄 | Time‑intensive to establish and maintain; training needed ⚡ | Excellent care coordination for complex patients; comprehensive view 📊 | Tertiary care, complex chronic disease management, academic centers 💡 | Organizes care by problem; enhances accountability and safety ⭐ |
| HPI (History of Present Illness) Template | Low–Moderate — focused narrative structure 🔄 | Can be time-consuming for detailed histories; efficient when templated ⚡ | Improves diagnostic accuracy and differential development 📊 | ED evaluations, initial consults, admissions where history drives diagnosis 💡 | Captures temporal symptom detail and pertinent negatives ⭐ |
| Chief Complaint + ROS Template | Low — simple to implement in most EHRs 🔄 | Variable; brief ROS is fast but exhaustive ROS is slower ⚡ | Broad symptom capture; supports coding and screening 📊 | New patient visits, annual exams, urgent care, specialty referrals 💡 | Captures patient's primary concern and systematic review of systems ⭐ |
| Physical Examination (PE) Template | Moderate — requires clinical skill and systematic approach 🔄 | Moderate time to perform; templates speed documentation ⚡ | Provides objective baseline data and detects abnormalities 📊 | Complete physicals, pre-op clearance, focused exams in clinic and hospital 💡 | Standardized objective findings; supports clinical decisions and legal record ⭐ |
| Problem List Template | Moderate — ongoing maintenance and reconciliation 🔄 | Requires regular updates; EHR integration improves efficiency ⚡ | Improves medication safety, care coordination, and quick status snapshot 📊 | Chronic disease management, transitions of care, discharge summaries 💡 | Centralized active problem tracking; aids reconciliation and prioritization ⭐ |
| Clinical Progress Note Template | Moderate — routine but disciplined documentation 🔄 | Time‑sensitive (daily notes); risk of copy‑forward if rushed ⚡ | Tracks clinical trajectory, justifies interventions, aids handoffs 📊 | Inpatient rounds, follow-ups, therapy sessions, nursing shifts 💡 | Chronological tracking of changes; supports continuity and quality metrics ⭐ |
| Assessment & Plan (A&P) Template | Moderate–High — requires clear clinical reasoning and prioritization 🔄 | Moderate time to create specific, measurable plans; benefits from numbered problems ⚡ | Yields actionable management, referrals, and measurable follow‑up outcomes 📊 | New diagnoses, acute exacerbations, chronic disease management, care planning 💡 | Synthesizes reasoning into concrete, time‑bound actions and follow‑up ⭐ |
From Templates to Transformation: The Future of Patient Documentation
Throughout this comprehensive guide, we've explored the foundational building blocks of effective, high-quality clinical documentation. From the structured logic of the SOAP note to the holistic overview provided by the Problem-Oriented Medical Record (POMR), each of the patient chart examples we analyzed serves a distinct yet deeply interconnected purpose. They are not merely forms to be filled out or boxes to be checked; they are the narrative frameworks that ensure continuity of care, facilitate clear and unambiguous communication between providers, and ultimately safeguard both patients and the practices that serve them.
Mastering these templates, whether for capturing a detailed History of Present Illness (HPI) or for outlining a concise and actionable Assessment and Plan (A&P), is a critical clinical skill. It is the process that transforms a collection of disjointed observations and patient statements into a coherent patient story, thereby enabling more accurate diagnoses and more effective, evidence-based treatment strategies. The true and enduring value of these structures lies in their proven ability to bring order, clarity, and consistency to the inherent complexity of human health.
Key Takeaways: From Structure to Strategy
Reflecting on the various templates and their applications, several core principles emerge as absolutely essential for excellence in modern healthcare documentation:
- Clarity is Paramount: Ambiguity has no place whatsoever in a patient chart. Each entry, from the Chief Complaint to the Physical Exam findings, must be precise, objective, and easily understood by any qualified member of the care team who might review it.
- Consistency Builds Continuity: The consistent use of standardized templates like the Problem List ensures that critical information is always captured and can be located in the same place within the record. This is absolutely vital for safely managing chronic conditions and nurturing long-term patient relationships.
- Efficiency Drives Quality: Inefficient documentation processes are not just an administrative burden; they steal valuable time directly from patient interaction and clinical reasoning. The goal is not just to be thorough, but to be thorough efficiently, leveraging well-designed templates and modern tools to streamline data entry without sacrificing quality.
However, understanding the theory behind these templates is only half the battle. The real-world challenge that clinics and hospitals face daily is populating them with accurate, timely, and complete information without succumbing to the overwhelming burden of administrative burnout. The relentless demand for detailed data entry is a primary contributor to clinician stress and can inadvertently pull focus away from the patient at the bedside.
Actionable Next Steps: Bridging the Gap with Technology
The future of clinical documentation isn't about finding a new, revolutionary template to replace the old ones. Instead, it’s about fundamentally revolutionizing the process of data collection itself. The core principles of good charting—clarity, consistency, and completeness—remain timeless, but the tools we use to achieve them are rapidly and excitingly evolving. This evolution of patient documentation is intricately linked to broader technological advancements that are shaping the future of physical therapy and all other medical specialties, where technology is increasingly being used to enhance both patient outcomes and provider efficiency.
To move your practice forward into this new era, consider these immediate, actionable steps:
- Standardize and Optimize Your Templates: Conduct a thorough review of your current EMR templates. Are they truly optimized for your most common visit types and workflows? A small, one-time investment in refining these digital forms can yield significant, cumulative time savings for your entire clinical team.
- Train Your Team on Documentation Best Practices: Ensure that everyone, from medical assistants and front-desk staff to nurses and physicians, understands the "why" behind each field in your preferred patient chart examples. Consistent training on documentation standards minimizes errors, improves data quality, and creates a more reliable patient record.
- Embrace Intelligent Automation: The most significant leap forward in conquering documentation burden lies in automating the data-gathering process. This is where AI-powered voice agents are making a truly transformative impact on clinical operations.
Imagine a system that can handle the entire patient intake conversation, ask relevant and adaptive clinical history questions based on the patient's chief complaint, and then intelligently parse that complex conversational information, populating the correct fields in your SOAP note or HPI template before the patient even steps into the exam room. This is no longer a futuristic concept; it is a practical, proven solution available to practices today. By automating these routine but critically important tasks, you empower your clinical staff to operate at the top of their license, focusing their invaluable expertise on diagnosis, treatment planning, and building meaningful patient rapport. This powerful synthesis of proven documentation structures and intelligent automation represents the next frontier in delivering exceptional, efficient, and sustainable healthcare.
Ready to eliminate documentation backlogs and free your staff for more meaningful work? See how Simbie AI uses advanced voice AI to automate patient intake and seamlessly populate your EMR with structured, accurate data from the patient chart examples you use every day. Transform your clinical workflow by visiting Simbie AI to learn more.

