Medical report formats are the essential blueprints clinicians use to document every aspect of patient care. Think of them as a shared, structured language that ensures clarity and continuity. Whether it’s a quick SOAP note documenting a routine check-up or a detailed discharge summary after a complex hospital stay, these standardized structures ensure that patient information is clear, consistent, and easily understood by the next provider. This isn’t just about administrative tidiness; it is a fundamental pillar of coordinating care, ensuring patient safety, and preventing costly medical errors. Mastering these formats is a non-negotiable skill for any healthcare professional dedicated to delivering the highest standard of care.
Why Clear Medical Report Formats Are Absolutely Essential
Imagine a pilot attempting to fly a commercial airliner without a pre-flight checklist. The process would be chaotic, unreliable, and dangerously prone to error. Standardized medical report formats serve the exact same purpose in the high-stakes environment of healthcare—they provide a reliable, predictable framework that eliminates ambiguity and ensures every member of the care team is operating from the same playbook.
Without a structured approach to documentation, critical details like medication allergies or significant past medical history can easily get buried in disorganized, free-text notes. A consulting specialist needs to locate a patient’s relevant history in seconds, not waste precious minutes deciphering convoluted paragraphs. An emergency room physician must be able to immediately grasp a patient’s current medications and allergies to make life-saving decisions. Standardized formats make this level of rapid comprehension possible, guaranteeing that the right information is in the right place, every single time. This structural integrity is the bedrock of safe and effective medical practice.
The Foundation of Patient Safety and Care Coordination
High-quality documentation is the backbone of safe, coordinated healthcare. When a patient navigates the complex journey from their primary care physician to a specialist, then to a hospital for a procedure, and finally to a rehabilitation facility, their medical record is the thread that tells their continuous story. Clear, consistent formats ensure that this story is coherent and easily followed by every provider involved, preventing dangerous gaps in care.
This has a direct and measurable impact on patient safety. For example, a well-written discharge summary that clearly outlines follow-up appointments, medication changes, and red-flag symptoms to watch for can dramatically reduce the likelihood of preventable hospital readmissions. Conversely, a sloppy or incomplete report can lead to misinterpreted physician orders, medication errors, or a missed critical diagnosis, with potentially devastating consequences for the patient.
Poor communication remains one of the most significant challenges in modern medicine. In fact, comprehensive studies from institutions like Johns Hopkins have shown that communication breakdowns contribute to up to 80% of serious medical errors. Standardized reporting is one of the most direct, effective, and universally applicable strategies to mitigate this risk head-on.
Reducing Ambiguity and Mitigating Legal Risks
Beyond the clinical setting, clear and standardized medical reports are your most robust defense from a legal and administrative standpoint. They create a definitive, time-stamped record of the care that was provided, which is crucial for justifying insurance claims, passing regulatory audits, and defending against potential legal challenges. Vague, incomplete, or disorganized notes are a significant liability and are incredibly difficult to defend if a patient’s care is ever called into question.
By consistently adhering to established medical report formats, you create documentation that is inherently:
- Objective: It focuses on verifiable facts, observations, and data, not subjective or speculative opinions.
- Comprehensive: It ensures that all essential components of a patient encounter, from history to plan, are systematically captured.
- Chronological: It presents a clear, logical timeline of events, diagnoses, treatments, and patient responses.
This guide is designed to be more than a simple list of definitions. We will delve into the real-world impact of exceptional documentation—exploring how it directly leads to better patient outcomes, streamlines team communication, and protects you and your practice from avoidable legal headaches. We will break down the most common and essential formats used in healthcare today, providing practical examples and best practices that you can apply immediately.
Common Medical Report Formats at a Glance
This table provides a quick, high-level summary of the most common medical report formats, their primary purpose, and where they are typically utilized within the clinical workflow.
| Format Type | Primary Purpose | Common Use Case |
|---|---|---|
| SOAP Note | To document a specific patient encounter with a structured thought process. | Daily progress notes, outpatient clinic visits, brief hospital updates. |
| H&P Report | To create a comprehensive baseline of the patient’s overall health status. | New patient admissions to a hospital, pre-operative evaluations, initial specialist visits. |
| Discharge Summary | To summarize a hospital stay and ensure safe continuity of care post-discharge. | A patient being discharged from a hospital, rehabilitation center, or skilled nursing facility. |
| Progress Note | To track a patient’s condition, response to treatment, and any changes over time. | Inpatient daily updates, follow-up visits for chronic disease management. |
| Referral Letter | To formally transfer care or request a consultation from another provider. | Sending a patient from a primary care physician to a specialist for expert opinion. |
| Operative Report | To provide a detailed, step-by-step account of a surgical procedure. | Mandatory documentation immediately following any surgical operation. |
| Consultation Report | To deliver a specialist’s findings, assessment, and recommendations back to the referring provider. | A specialist’s formal response to a referral request from another clinician. |
Each of these distinct formats serves a specific, vital function in the ecosystem of patient care. In the following sections, we will dive deep into the structure, components, and best practices for each one, exploring exactly when and how to use them effectively to achieve clinical excellence.
The Four Foundational Medical Report Formats
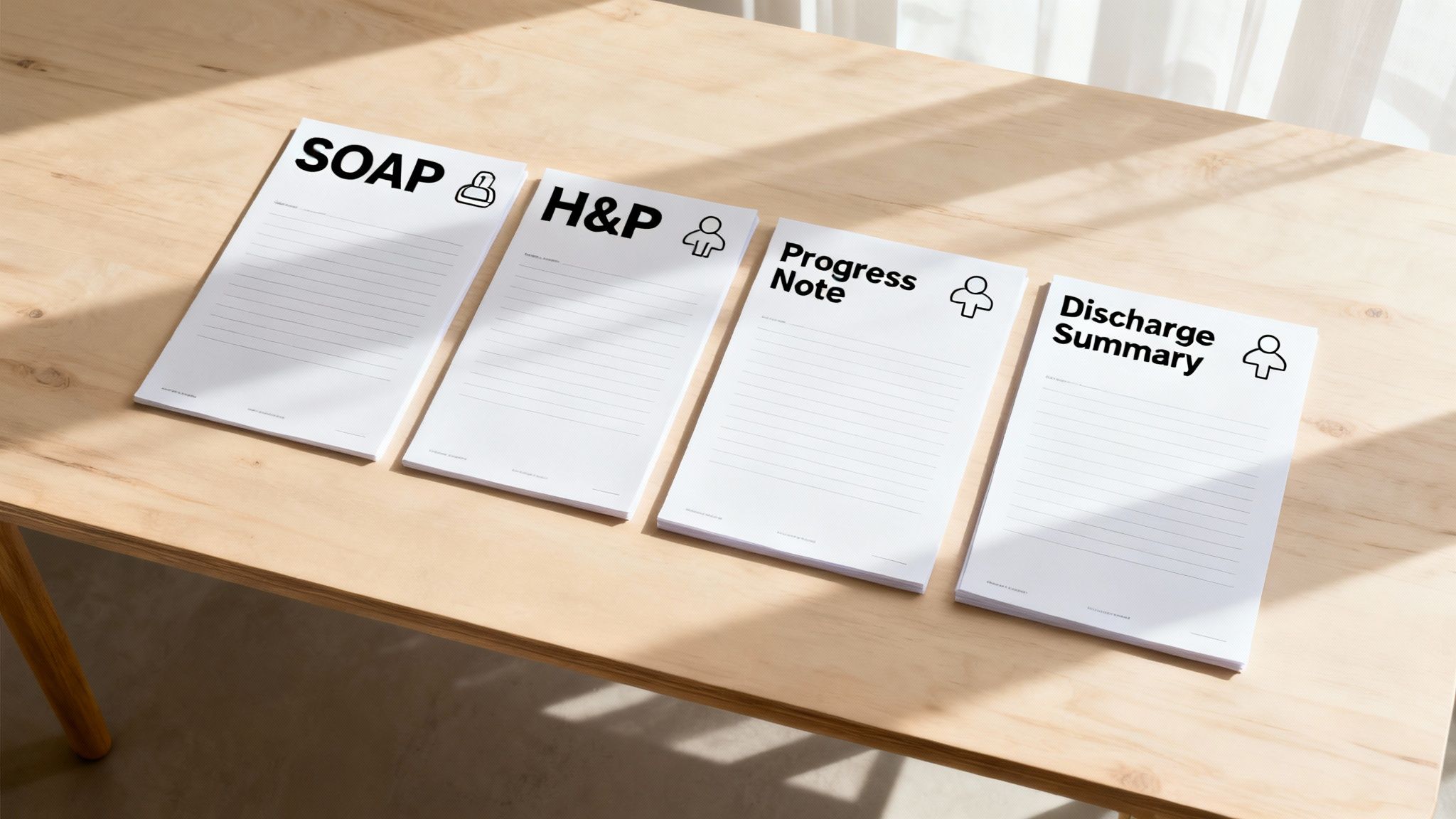
While the field of healthcare generates an endless stream of complex paperwork, a few core report formats stand as the absolute pillars of clinical communication and documentation. If you want to tell a patient’s story clearly, accurately, and effectively, you must achieve mastery of these four fundamental structures. Each one is meticulously designed for a specific purpose, capturing a unique and critical moment in the patient’s ongoing care journey.
Think of them as different, specialized tools in a clinician’s toolbox. You wouldn’t use a hammer to turn a screw, and you wouldn’t use a wrench to make a precise incision. In the same way, you wouldn’t write a quick, daily progress note when what the situation truly demands is a comprehensive history and physical exam that establishes a patient’s baseline. Knowing precisely which format to use—and when to use it—is the key to efficient, accurate, and defensible medical documentation.
These four essentials are the SOAP note, the History and Physical (H&P), the Progress Note, and the Discharge Summary. Let’s dig into the specific components and strategic importance of what makes each one tick.
The SOAP Note: A Detective’s Case File
The SOAP note is arguably the most common, versatile, and frequently used format in all of medicine. It provides a clean, logical, and structured method for documenting a single patient encounter, making it perfect for everything from a routine check-up in an outpatient clinic to daily rounds on a busy hospital ward. The true power of the SOAP note lies in how it mirrors the natural, deductive flow of a clinician’s thinking process.
Imagine a detective meticulously building a case. A SOAP note functions in precisely the same way, organizing information into a coherent narrative:
- Subjective (S): This is the patient’s story—the “clues.” It encompasses everything the patient, their family, or their caregiver tells you. This includes the chief complaint, the history of the present illness, and a review of relevant symptoms. The goal is to capture their personal account, ideally using their own words to convey their experience accurately.
- Objective (O): Now for the hard, verifiable evidence. This section is reserved exclusively for the objective facts you gather during the encounter. This includes vital signs (blood pressure, heart rate, temperature), physical exam findings, laboratory results, and imaging reports. Anything measurable, observable, and reproducible goes here.
- Assessment (A): This is where the detective forms a hypothesis based on the evidence. Synthesizing the subjective clues and the objective data, you will list your primary diagnosis. This section should also include any other potential diagnoses you are considering (your differential diagnoses), ranked in order of likelihood.
- Plan (P): Finally, the action plan. This section clearly outlines the next steps for the patient’s care. Are you ordering additional diagnostic tests? Prescribing or adjusting medication? Referring the patient to a specialist? Scheduling a follow-up visit or providing the patient with new instructions for self-care? Every component of the immediate plan is documented here.
This intuitive structure makes it incredibly easy for any provider on the care team to pick up a patient’s chart and immediately understand what is going on, why a certain diagnosis was made, and the rationale behind the chosen treatment plan. If you’re looking for a solid starting point to standardize your documentation, this free SOAP note template can help you internalize and master the structure.
The History and Physical: A Complete Patient Blueprint
If a SOAP note is a single, focused snapshot of a patient’s condition at one point in time, the History and Physical (H&P) is the patient’s complete health blueprint. This is a far more detailed and comprehensive document, typically created when a patient is first admitted to the hospital, becomes a new patient at a practice, or is being evaluated before a major surgical procedure. The entire goal of the H&P is to establish a thorough and accurate baseline of the patient’s health.
An H&P is a deep dive, methodically documenting every facet of a patient’s medical life to guide all future diagnostic and treatment decisions.
The H&P is the cornerstone of any hospital admission or new patient workup. It provides the full context needed for accurate diagnosis and safe treatment, ensuring no critical piece of the patient’s past is overlooked. A hastily prepared or incomplete H&P can directly lead to diagnostic errors, medication mistakes, and unsafe care.
Key components of a comprehensive H&P always include:
- Chief Complaint: The primary reason the patient is seeking medical care, often stated in their own words.
- History of Present Illness: A detailed narrative of the current problem, including onset, duration, severity, and associated symptoms.
- Past Medical History: A thorough record of previous illnesses, chronic conditions, hospitalizations, and surgeries.
- Medications and Allergies: A complete and verified list of all current medications (prescription, over-the-counter, supplements) and any known allergies to avoid dangerous adverse reactions.
- Social and Family History: Information about lifestyle factors (e.g., smoking, alcohol use) and any significant genetic or familial health risks.
- Review of Systems: A systematic, head-to-toe inventory of symptoms across all major body systems to catch any overlooked issues.
- Physical Examination: The clinician’s objective findings from the hands-on physical exam, organized by body system.
- Assessment and Plan: The initial differential diagnosis and the proposed course of action for further testing and initial treatment.
Progress Notes: The Ongoing Story
While the H&P sets the initial stage, Progress Notes are the documents that tell the continuing story of a patient’s journey through a hospital stay or their long-term management of a chronic condition. These notes are frequently structured like abbreviated SOAP notes (sometimes called “SOAP-I-ME” to include interventions, monitoring, and education), but their primary focus is squarely on tracking changes, updates, and responses to treatment over time.
Think of Progress Notes as the daily entries in a ship’s log. They chart the patient’s course, meticulously noting improvements, setbacks, responses to medication, and any new issues that arise. This continuity of information is absolutely critical, especially in a hospital setting where care is handed off between shifts or among different providers on a team. A physician starting their shift can quickly read the last few progress notes and get fully up to speed on a patient’s status in a matter of minutes, ensuring seamless and safe care.
The Discharge Summary: A Handover for Safe Passage
The Discharge Summary is the final, crucial chapter of a hospital stay. Its entire purpose is to ensure a safe, smooth, and well-coordinated transition of care from the hospital back to the patient’s primary care provider, a rehabilitation facility, or their home. This is one of the most important documents for preventing hospital readmissions, which are not only financially costly for the healthcare system but also represent significant risks and setbacks for patients.
This report comprehensively recaps the entire hospital course, from the moment of admission to the moment of discharge. It serves as the ultimate handover document, providing clear and actionable instructions for what must happen next. A high-quality discharge summary always includes:
- Reason for Hospitalization: A clear statement of what brought the patient into the hospital.
- Significant Findings: A summary of key lab results, imaging findings, and final diagnoses.
- Hospital Course: A concise narrative of the major treatments administered and the patient’s response to them.
- Discharge Condition: A description of the patient’s health status at the time they left the hospital.
- Discharge Medications: A clear, reconciled list of all medications the patient should be taking, explicitly highlighting any changes from their home medication regimen.
- Follow-Up Instructions: Details on upcoming appointments, any pending test results to watch for, and specific instructions regarding diet, activity restrictions, or self-care.
When utilized correctly and diligently, these four foundational medical report formats work in concert to create a complete, cohesive, and clear patient narrative that enhances communication and elevates the standard of care.
Specialized Reports for Specific Clinical Needs
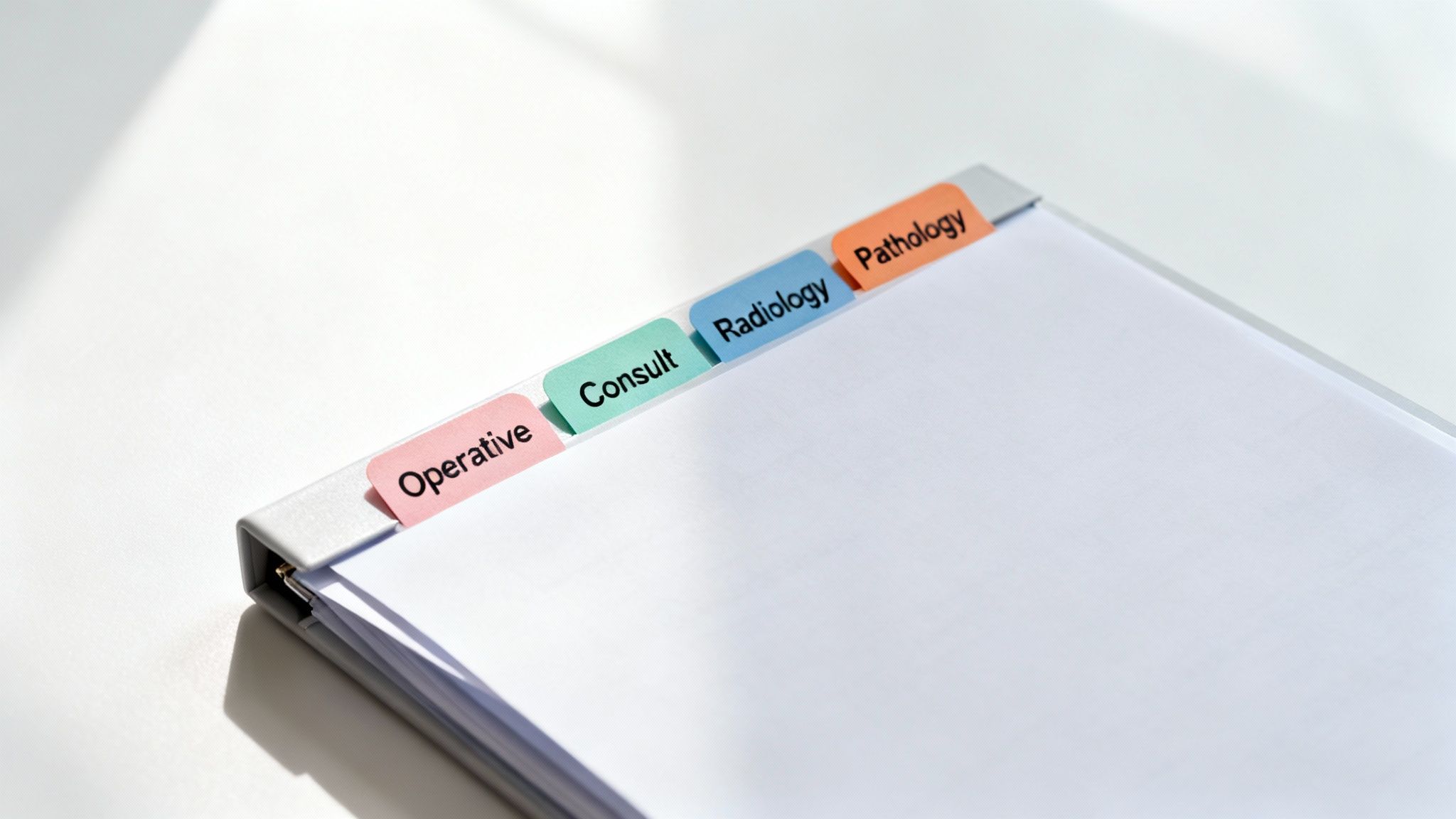
While the four foundational report formats cover the majority of daily documentation needs, modern medicine relies on a suite of specialized tools designed for very specific jobs. These reports are purpose-built to capture the precise, granular information required in unique clinical situations, such as surgery, diagnostic imaging, or specialty consultations. They are the high-precision instruments of medical reporting, where detail and structure are paramount.
Think of it in this context: a family physician might effectively use a versatile multi-tool (like a SOAP note) for most routine check-ups and follow-ups. A surgeon, however, needs a scalpel—a tool designed for a single, critical purpose. A radiologist requires a specialized viewer and a rigid reporting structure to interpret complex images. These unique report formats fill those distinct roles, ensuring every last critical detail is captured with the appropriate level of clarity and specificity.
The Operative Report: A Surgeon’s Detailed Narrative
The moment a patient is taken into the operating room, a new and critical chapter in their care begins, and the Operative Report serves as its official, unalterable record. This is not a brief summary; it is a meticulous, step-by-step account of a surgical procedure, typically dictated by the primary surgeon immediately after the operation concludes. It functions as a detailed narrative explaining exactly what was done, what was found, and how the procedure concluded, from the initial incision to the final stitch.
As both a critical legal document and an essential clinical tool, the Operative Report is indispensable. It guides post-operative care decisions, provides the justification for billing and coding, and acts as a vital reference for any future procedures the patient may require.
Here’s what you will always find within a standard Operative Report:
- Pre-operative and Post-operative Diagnoses: The reason the surgery was necessary and the final diagnosis confirmed by the procedure.
- Procedure Performed: The official, standardized name of the operation.
- Surgeons and Assistants: A complete roll call of every clinician who participated in the procedure.
- Anesthesia Details: The type of anesthesia used (e.g., general, spinal) and a note on how the patient tolerated it.
- Findings: A play-by-play description of what the surgeon observed and discovered during the operation. This includes the state of the organs and any unexpected abnormalities.
- Procedure Description: The most detailed section, providing a chronological, step-by-step account of every surgical action taken.
- Specimens Removed: A record of any tissue, fluid, or other samples that were removed and sent to the pathology lab for analysis.
- Estimated Blood Loss: A crucial metric for monitoring the patient’s hemodynamic stability and recovery.
This strict, universally accepted structure guarantees that any other provider—from a post-op nurse to another surgeon years later—can pick up the report and understand exactly what happened in the OR, which is absolutely essential for managing a patient’s short-term recovery and long-term health.
Consultation Reports and Referral Letters
Patient care is rarely a linear process managed by a single provider. Often, a primary care physician requires an expert opinion from a specialist, or a patient’s care must be formally handed off to another clinician for specialized treatment. This is where Consultation Reports and Referral Letters step in, serving as the formal, documented bridge of information between different providers.
A Referral Letter is the document that initiates this process. It is a concise yet comprehensive summary of the patient’s case, clearly stating the reason for the referral and the specific clinical question that needs to be answered by the specialist. It provides just enough context—the “why” and “what” of the patient transfer—for the next clinician to hit the ground running without having to reconstruct the patient’s entire history from scratch.
The Consultation Report is the specialist’s formal response. After seeing and evaluating the patient, the specialist drafts this report and sends it back to the original referring physician. It meticulously outlines their findings from the history and exam, their expert assessment of the situation, and their specific recommendations for treatment or further testing. This report effectively closes the communication loop, ensuring that care remains coordinated and that the primary physician is equipped to implement the specialist’s advice.
A well-crafted consultation report is not just a document; it is a dialogue between clinicians. It should clearly and directly answer the referring physician’s questions and provide an actionable, evidence-based plan. This prevents the fragmentation of care and ensures the patient benefits from collaborative, multidisciplinary expertise.
Radiology and Pathology Reports: The Language of Precision
When a definitive diagnosis hinges on the interpretation of a tissue sample or a sophisticated imaging scan, there is absolutely zero room for ambiguity or error. Radiology Reports and Pathology Reports are two of the most rigidly structured and standardized medical report formats for precisely this reason—they are built for absolute diagnostic precision and clarity.
A Radiology Report, which provides the official interpretation of images like X-rays, CT scans, and MRIs, almost always follows a strict, predictable pattern:
- Technique: A description of how the image was acquired (e.g., “CT scan of the abdomen with and without intravenous contrast”).
- Findings: An objective, detailed, and systematic description of what the scan shows, avoiding any interpretation.
- Impression: The radiologist’s final diagnosis or conclusion based on the findings, presented as a clear and concise summary.
In the same way, a Pathology Report analyzes tissue samples under a microscope to provide a definitive diagnosis for conditions like cancer. It describes cellular characteristics in minute, standardized detail, often providing a grade and stage for malignancies.
Both of these specialized report types use standardized, universal terminology so that their conclusions can be understood without ambiguity by any clinician, anywhere in the world. The diagnostic stakes are simply too high for anything less. These reports must prioritize objective data and clear, final conclusions above all else, making them cornerstones of modern evidence-based medicine. For a closer look at this kind of specialized documentation, a complete guide to teleradiology services and reporting offers some great real-world insights into this field.
How Chronological Reporting Works in Medico-Legal Cases
When a patient’s health and medical history become the centerpiece of a legal proceeding or an insurance claim, standard clinical reports often fall short. Lawyers, insurance adjusters, and judges are not just looking for isolated snapshots of care; they need to understand the entire story as it unfolded over time, from the initial incident to the final prognosis. This is where the medical chronology shines. It is a specialized type of report designed to transform a potentially chaotic and voluminous collection of medical records into a clear, linear, and easy-to-understand narrative.
Think of it this way: a SOAP note is a single scene in a movie, and a discharge summary might be the final act. A medical chronology, however, is the full, unabridged film. It meticulously lines up every single appointment, diagnosis, prescription, lab result, and procedure in the exact order it happened. This process creates a powerful, easy-to-follow timeline that makes sense even to individuals who have no background in the medical field.
This format is absolutely essential in personal injury claims, workers’ compensation disputes, and medical malpractice lawsuits—any situation where proving a clear and undisputed sequence of events is the key to building a successful case.
Building a Coherent Story from Scattered Records
The process of creating a comprehensive medical chronology is painstaking and detail-oriented work. It begins with the monumental task of gathering every single shred of a patient’s medical history, which can mean sifting through hundreds or even thousands of pages of documents from various providers. This can include everything from handwritten physician’s notes and complex lab results to MRI reports, hospital billing codes, and physical therapy records. The ultimate goal is to distill all of that disparate information into one unified, accessible, and chronologically sound document.
Essentially, the process involves stripping away the clinical complexity and medical jargon to present the core facts in a straightforward manner.
The workflow for creating a medical chronology typically breaks down into three main steps:
- Record Collection and Organization: The first step is to compile and organize every relevant medical document from every single provider the patient has seen related to the case.
- Data Extraction and Review: Next, a trained reviewer meticulously goes through each page to identify and pull out all the key events, dates, diagnoses, treatments, and other important details from each record.
- Summarization and Sequencing: Finally, all of this extracted information is summarized in plain, accessible English and arranged in perfect chronological order, creating a seamless narrative timeline.
This highly structured process transforms what is often a chaotic and overwhelming paper trail into an organized, evidence-based story that can hold up under the scrutiny of a courtroom or during high-stakes insurance negotiations.
The Critical Role of Chronology in Legal and Insurance Claims
In the legal and insurance industries, the medical chronology is a heavy-hitting tool, especially for personal injury cases. A well-prepared report lays out the patient’s entire medical journey on a strict, date-based timeline, highlighting crucial events such as the date of injury, the subsequent diagnoses, the various treatments they received, and the final medical prognosis. The process involves taking massive volumes of data and trading complex medical terminology for straightforward, factual summaries that a lawyer can actually use to build their case.
Because this is such a labor-intensive and specialized task, many legal teams and insurance companies rely on professional medical chronology review services to ensure accuracy and efficiency. If you want to get a better feel for the intricacies involved in this process, you can learn more about how to prepare a medical chronology report that keeps a legal or insurance claim on a successful track.
A well-crafted chronology doesn’t just list events; it reveals critical patterns and relationships. It can draw a straight, undeniable line from a specific accident to the medical treatments that followed, or it can expose unexplained gaps in care that might point toward potential negligence. That kind of narrative clarity can completely change the outcome of a case.
Making Complex Medical Histories Make Sense
Ultimately, the real strength and value of a medical chronology lie in its simplicity and clarity. It is a document built from the ground up to be understood by judges, lawyers, and jury members who do not have a medical degree. By translating a complex and often convoluted clinical history into a simple, clear, and logical timeline, it provides legal teams with the solid factual foundation they need to build stronger arguments, depose witnesses effectively, and present their evidence in a compelling manner.
This clarity is vital for achieving legal and financial accountability. It ensures that critical decisions are based on a full, accurate, and unbiased picture of what the patient went through. In many medico-legal cases, the medical chronology is not just another piece of paper—it is often the single most influential document that provides the factual bedrock for a just and equitable outcome.
Integrating Report Formats with Modern EHR Systems
Think of standardized medical report formats as the timeless architectural blueprints for documenting patient care. The Electronic Health Record (EHR) system, then, is the modern, digital construction site where these well-established plans are brought to life with unprecedented speed and efficiency. Today’s EHR platforms take the foundational principles of a SOAP note, an H&P, or a discharge summary and embed them directly into the daily grind of clinical practice, making documentation faster, more consistent, and more reliable than ever before.
Instead of scribbling notes on a physical chart, clinicians now leverage powerful digital tools like templates, macros, and smart phrases to construct comprehensive reports in a fraction of the time. This doesn’t just save precious minutes in a busy day; it also enforces a crucial level of consistency in documentation, ensuring that vital data points are captured in the same standardized way, every single time, by every provider in the organization.
The Double-Edged Sword of Digital Templates
The most significant advantage of bringing medical report formats into an EHR is undoubtedly the massive efficiency boost gained from using templates. A well-designed digital template for a History and Physical (H&P), for example, acts as an invaluable guide, systematically walking a clinician through every essential section so that nothing important gets overlooked. It functions as a powerful safety net against incomplete or disorganized documentation.
However, there is a well-known catch. Over-reliance on these templates can lead to a phenomenon known as “note bloat”—a common and frustrating issue where reports become crammed with generic, auto-filled, or copied-and-pasted text that ultimately obscures the actual patient story. The true art of modern clinical documentation is striking a delicate balance: using the template as a reliable framework but always taking the time to tailor it with the specific, human details of the unique patient in front of you.
It’s a frequent and valid complaint you’ll hear from clinicians across all specialties: EHRs can sometimes feel as though they were designed for billing and coding first, and patient care second. The only way to combat this is for practices to proactively customize their workflows and templates to put clear, clinically useful, and patient-centric documentation back in the driver’s seat.
Practical Tips for Making Your EHR Work for You
To prevent digital templates from becoming more of a hindrance than a help, healthcare practices need to be willing to roll up their sleeves and invest time in customizing their EHRs. The overarching goal is to make the technology serve your clinical workflow, not the other way around.
- Build Your Own Bespoke Templates: Create highly specialized templates for the most common conditions, procedures, and patient complaints you see day in and day out. This allows you to pre-populate the predictable information while leaving ample, clearly defined space for your unique findings and assessments.
- Master Smart Phrases and Macros: Become proficient in using macros or “dot phrases” to instantly insert frequently used blocks of text. For instance, typing a shortcut like “.normalexam” could instantly populate a full paragraph describing a standard physical exam, which you can then quickly tweak as needed to reflect any specific abnormalities.
- Prune Your System Regularly: At least every few months, conduct a thorough review of your existing templates, smart phrases, and order sets. Get rid of outdated options, consolidate redundant fields, and refine your macros to combat note bloat and keep your documentation as sharp and concise as possible.
Making these kinds of strategic, ongoing tweaks is a huge part of successful EMR system integration, a complex topic that we cover in much more detail in our dedicated, in-depth guide.
What’s Next? AI and the Future of Smarter Reporting
A new wave of technology is on the horizon, poised to completely revolutionize how we interact with medical report formats within our EHRs. Artificial intelligence (AI) and natural language processing (NLP) are already demonstrating incredible potential for automating and augmenting some of the most tedious and time-consuming documentation tasks.
Imagine this future workflow: an NLP algorithm listens ambiently to a natural, dictated note or a doctor-patient conversation and automatically structures that unstructured speech into a perfectly formatted SOAP note or a detailed medical chronology. That is the transformative power of this technology—it can turn a simple conversation into structured, searchable, and analyzable data that can unlock powerful clinical insights and free up clinicians to focus more on patient care.
As EHR adoption continues to grow—with well over 85% of U.S. hospitals and more than 75% in Western Europe now using them—our ability to rapidly pull together accurate and comprehensive medical histories has improved dramatically. This fundamental shift from paper to digital has slashed the time needed for complex tasks like medical chronology preparation from weeks down to just days or even hours. This newfound efficiency is fueling a rapidly expanding global market for medical chronology services, which is expected to grow by approximately 5% annually.
At the end of the day, the ultimate goal is to make technology a true and seamless partner in the delivery of patient care. By thoughtfully integrating smarter workflows, customized templates, and emerging AI-powered tools, we can significantly elevate the quality and consistency of our medical reports, which leads directly to better-informed clinical decisions and, ultimately, better outcomes for our patients.
Best Practices for Effective Medical Reporting
Creating a truly great medical report is about much more than simply filling out a form or checking boxes in an EHR. It’s about meticulously building a document that actively protects your patient, streamlines communication across the care team, and provides a clear, defensible record of your clinical decision-making. Think of it less as a burdensome administrative chore and more as a powerful clinical tool that directly impacts patient safety and quality of care.
The best medical reports manage to achieve the delicate balance of being both concise and comprehensive. You must include every clinically critical detail without burying the most important information in a sea of irrelevant text. The goal is to tell a clear, direct, and unambiguous story that another provider, who may be unfamiliar with the patient, can pick up and understand in a matter of seconds.
Prioritize Clarity and Objectivity Above All
Always, without exception, stick to objective and descriptive language. Your primary job in documentation is to describe what you see, hear, and measure—not what you guess, assume, or infer. Instead of writing a subjective statement like “patient seems anxious,” document the objective facts that led to that conclusion: “patient is fidgeting, wringing hands, heart rate is 110 bpm, and reports feeling worried and unable to sleep.” Being specific and factual leaves no room for dangerous misinterpretation by other members of the care team.
Another huge point of emphasis is to ditch dangerous or unapproved abbreviations. Using shortcuts is tempting, especially on a busy day, but an unapproved, ambiguous, or unclear acronym is a well-known recipe for serious medical errors. If your hospital or practice has an officially approved abbreviation list, follow it to the letter. If you are ever in doubt, the safest and most professional course of action is always to just write it out.
Never put off your documentation. Timeliness is a non-negotiable component of high-quality reporting. Finishing your notes immediately after a patient encounter ensures that the information is fresh, accurate, and complete. A report written days or even hours after an appointment is far more likely to contain factual errors or critical missing details.
Tailor the Report to Its Intended Audience
Always remember who you’re writing for. The content and focus of your report should be tailored to its intended reader. A referral letter to a cardiologist, for instance, needs to be focused and concise, highlighting the specific clinical question you need them to answer. On the other hand, a report prepared for legal or insurance purposes, such as a medical chronology, must be incredibly detailed, meticulously organized, and written in plain language that a non-clinician can easily understand.
When done correctly, using standardized medical report formats can have a tangible positive impact on administrative processes. For example, clear and well-organized reports can actually speed up insurance claim processing by as much as 30%. It makes the critical data easy for reviewers to find, which helps patients get the compensation or insurance settlements they are entitled to much faster.
For a deeper dive into the principles of creating clear, effective, and audience-aware reports, check out these excellent guidelines for crafting comprehensive diagnostic evaluation report letters.
A Quick Checklist for Avoiding Common Documentation Pitfalls
To keep your medical reports clean, accurate, and professional, be vigilant in watching out for these common and easily avoidable slip-ups:
- Careless Copy-Paste Errors: It’s easy to overuse the copy-forward feature in an EMR, but doing so without careful review can pull outdated or flat-out wrong information into a patient’s current chart, leading to serious errors.
- Forgetting to Document Patient Education: Always make a specific note of what you taught the patient, whether they demonstrated understanding of the information, and what educational handouts or resources you provided them with.
- Incomplete Medication Reconciliation: Failing to meticulously reconcile a patient’s medications at every single visit is consistently identified as one of the single biggest causes of preventable patient harm.
Internalizing these best practices is a cornerstone of any effective clinical documentation improvement (CDI) program. It transforms your reports from simple administrative records into powerful, active tools that boost patient safety, reduce medical errors, and make care transitions seamless and safe.
Your Top Questions About Medical Reports, Answered
Let’s be honest, navigating the complex and ever-evolving world of clinical documentation can often feel like trying to solve a maze. You are not alone if you have questions about the nuances of different report formats and best practices. Here are some clear, straightforward answers to the questions that healthcare professionals ask most often.
What Is the Single Most Common Medical Report Format I’ll See?
Hands down, the most ubiquitous and frequently utilized medical report format is the SOAP note. Think of it as the fundamental workhorse of clinical documentation, employed everywhere from bustling primary care clinics for routine visits to specialized hospital wards for writing daily progress notes on inpatients.
Its simple, logical Subjective, Objective, Assessment, and Plan structure is precisely what makes it so powerful and universally adopted. It creates a shared mental model and a universal language that allows any provider, regardless of their specialty, to get up to speed on a patient’s current status almost instantly. For this reason, it remains the undisputed backbone of day-to-day patient care documentation across the globe.
How Has the Rise of Telehealth Changed How We Write Reports?
The widespread adoption of telehealth isn’t necessarily inventing entirely new report formats, but it is certainly prompting important tweaks and additions to the ones we already use. A SOAP note for a virtual visit, for example, will look almost identical to one for an in-person appointment, but it will contain a few key differences. For instance, the ‘Objective’ section will need to explicitly state that the physical examination was conducted visually via video and should mention any specific limitations that came with not being physically in the room with the patient (e.g., inability to palpate the abdomen).
There are also a few extra pieces of administrative and legal information that you must include in telehealth documentation to keep everything clear, compliant, and billable.
When documenting any telehealth visit, you absolutely need to record the patient’s explicit consent for the virtual appointment, the specific technology platform you used (like Doximity, Zoom for Healthcare, or a native EMR portal), and a statement confirming where the patient was physically located during the visit to comply with state licensing laws. The best EMRs are already adding dedicated, structured fields to make capturing this essential information easy and routine.
Is It Okay to Use Abbreviations in My Clinical Notes?
The short answer is yes, you can use them, but you must be incredibly careful and disciplined. Abbreviations are a classic double-edged sword in medicine; they can save a significant amount of time during documentation, but they can also lead to serious and preventable medical errors if they are misinterpreted by another member of the care team.
Most modern healthcare systems maintain an official, approved list of abbreviations to prevent this kind of dangerous confusion. Your first rule should be to stick to that list without deviation. Furthermore, The Joint Commission, a key accrediting body, publishes an official “Do Not Use” list of abbreviations that are considered too risky to ever be used in clinical documentation. If you have even a shadow of a doubt about whether an abbreviation is appropriate or clear, the safest and most professional choice is always to write the full term out.
What’s the Real Difference Between an EMR and an EHR?
People use these two terms interchangeably all the time, but they don’t actually mean the same thing. The critical distinction between them is all about how far the patient’s information is designed to travel and be shared.
- An EMR (Electronic Medical Record) is a digital version of a patient’s chart that is created and used within one single practice or healthcare organization. It contains the story of a patient’s care within your four walls. It is not designed to be easily shared with outside providers.
- An EHR (Electronic Health Record) represents the bigger, more comprehensive picture. It is designed from the ground up to pull in records from multiple doctors, hospitals, labs, and other organizations to create a single, unified, and complete health history for a patient. An EHR is built for interoperability and is designed to follow the patient wherever they go for care, from their family doctor to the hospital to a specialist across the country.
Are routine administrative tasks bogging down your skilled clinical team and leading to burnout? Simbie AI is a clinically-trained voice AI that expertly handles patient intake, scheduling, insurance verification, and even prescription refills, all while integrating seamlessly with your existing EMR. Give your staff a much-needed break from administrative overload and dramatically improve the patient experience at the same time. Visit Simbie AI to learn more.

