Why Medical Call Centers Are Transforming Healthcare

Imagine it’s 3 AM. Sarah is worried because her elderly father has developed some concerning symptoms. Instead of rushing to the emergency room in a panic, she dials her healthcare provider's 24/7 support line. A trained professional answers, calmly assesses the situation, offers clear advice, and helps her figure out what to do next. This entire, crucial interaction is made possible by a modern medical call center.
These communication hubs are no longer the simple answering services of the past. Today, they act as the central nervous system for healthcare organizations, connecting patients with the exact care they need, when they need it. They are the essential bridge between a patient's question and a provider's solution, handling everything from urgent medical advice to routine appointment scheduling and prescription refills. For many people, the call center is their first and most frequent point of contact, shaping their entire perception of a healthcare system.
The pressure on these centers is enormous. A single healthcare call center can field an average of 2,000 calls every day. During busy periods, staffing often covers only about 60% of what’s needed to manage the volume. This gap leads to an average hold time of 4.4 minutes, a long wait when you're concerned about your health. The consequences are significant, as patients who have a poor call experience are four times more likely to find a new provider. You can see more detailed healthcare call center statistics and trends here.
This challenging environment shows why effective and empathetic communication isn't just a bonus—it's a necessity. Trust and continuity of care begin with that very first phone call. To improve this critical touchpoint, forward-thinking providers are investing in better systems and workflows. Mastering these interactions is a key part of building patient loyalty and ultimately, improving health outcomes. Learn more about building effective healthcare communication strategies in our guide.
Essential Functions That Drive Patient Success
Think of a medical call center not as a simple answering service, but as the central nervous system of a healthcare practice. It’s the hub that connects patients to the care they need, coordinating a multitude of moving parts to ensure everything runs smoothly. These centers are more than just a convenience; they are vital command posts that directly influence patient outcomes and provide a sense of security for individuals and their families.
Core Patient Support Services
The real value of a medical call center becomes clear when you look at its daily responsibilities. These are not just administrative chores; they are the critical touchpoints where trust is built and patient care is coordinated effectively. Key functions include:
- Intelligent Appointment Scheduling: This is far more than just finding an open slot on a calendar. Agents use smart reminder systems and proactive scheduling to minimize no-shows. By filling last-minute cancellations, they also ensure a provider's schedule is full, improving access to care for everyone.
- Clinical Triage Support: When a patient calls with symptoms, trained staff follow strict medical protocols to assess the situation. They can skillfully determine the difference between a minor issue that can wait for a regular appointment and a true emergency that requires immediate medical attention.
- Prescription and Insurance Management: Call center agents help patients avoid dangerous gaps in their medication by managing refill requests. They also perform insurance verifications to clarify coverage details, which helps prevent unexpected bills and reduces financial anxiety for patients.
- After-Hours Support: Health concerns don’t stick to a 9-to-5 schedule. Providing a calm, knowledgeable voice after the clinic has closed gives immense peace of mind to patients and caregivers who are dealing with an unexpected health issue.
The table below breaks down these key medical call center functions, highlighting their complexity, impact on patients, and the specific skills needed to perform them well.
Medical Call Center Core Functions Comparison
Comparison of different medical call center functions, their complexity levels, and impact on patient satisfaction
| Function | Complexity Level | Patient Impact | Required Skills |
|---|---|---|---|
| Appointment Scheduling | Low to Medium | High | Strong organizational skills, attention to detail, clear communication. |
| Clinical Triage Support | High | Critical | Adherence to medical protocols, empathy, quick decision-making, basic clinical knowledge. |
| Prescription/Insurance Help | Medium | High | Meticulous accuracy, knowledge of insurance terminology, problem-solving. |
| After-Hours Support | Medium to High | Critical | Calm demeanor under pressure, broad medical knowledge, excellent listening skills. |
As the comparison shows, the roles within a medical call center demand a diverse set of skills. While some tasks are administrative, others like clinical triage have a direct and serious effect on patient safety. A high-performing team masters both the organizational and the empathetic aspects of these jobs.
Executing these functions effectively is the foundation of a successful patient experience. The following infographic shows how these services typically break down by call volume.
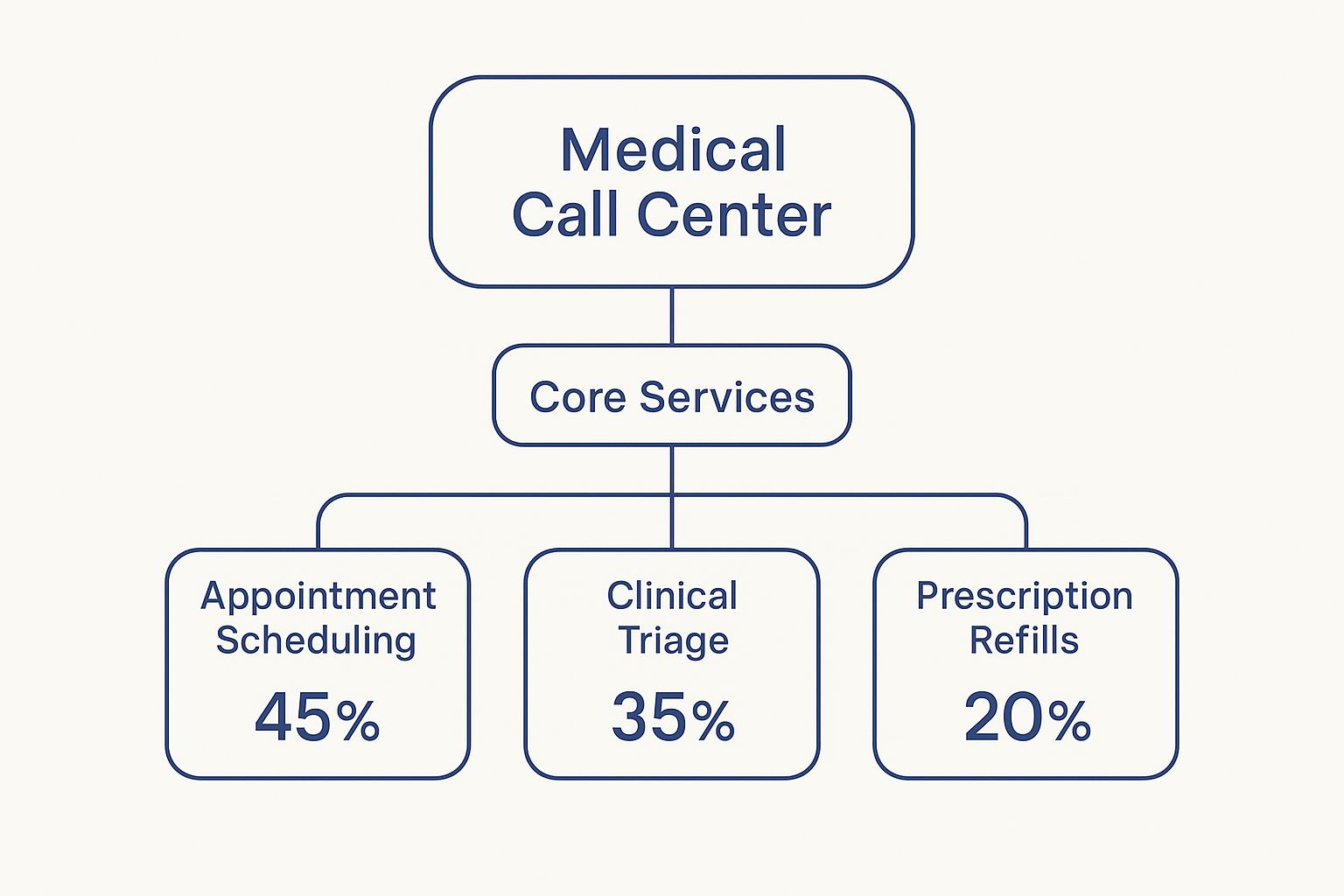
The data reveals that administrative tasks, such as managing appointments, account for a significant 45% of all calls. This highlights a major area where efficiency and empathy can make a huge difference. When every interaction is handled with care, patient confidence in their provider grows. You can discover tips for boosting patient happiness in our related guide.
Three Proven Models: Finding Your Healthcare Match

Selecting the right model for your medical call center is a bit like a doctor prescribing a treatment. The perfect solution for one practice might not be right for the next. Each approach has its own strengths and weaknesses, and the best choice hinges on your clinic’s unique circumstances, budget, and the community you serve.
The In-House Team
Think of an in-house team as building a new, dedicated department right inside your own facility. This approach gives you maximum control over everything—from hiring and training to shaping the service culture. Your team becomes deeply familiar with your providers, procedures, and patients, creating a natural extension of your practice's care.
For example, a local pediatric clinic could train its own staff to handle calls from worried parents with a specific tone and knowledge base that reflects the clinic's values. The flip side, however, is the significant upfront and ongoing investment. You're responsible for salaries, benefits, technology, and management, which means overhead can be a major factor.
The Outsourced Partner
Choosing an outsourced solution is like bringing in a team of specialists to handle a specific job. You gain instant access to trained agents and ready-to-go technology, which lets you get up and running quickly without a large capital outlay. These partners are pros at managing calls efficiently and can easily scale up or down based on your needs.
The primary trade-off is a degree of separation from your practice's day-to-day culture. While professional, an external team might not have the same instinctual grasp of your specific patient community or internal workings. This can sometimes affect the personal touch that patients feel when they call.
The AI-Powered Platform
The third option is to use an AI-powered platform, which acts as a tireless digital assistant for your practice. These systems can manage a wide range of patient interactions automatically, providing a consistent experience every time. They are particularly good at handling routine tasks, which frees up your human staff to focus on patients with more complex or urgent needs.
Key advantages include:
- 24/7 availability for patients calling after hours.
- Immediate handling of high call volumes without wait times.
- Consistent, accurate information based on your practice's protocols.
The main consideration here is ensuring the technology is set up to be helpful and not frustrating. It's crucial to design the system to preserve the warmth and empathy patients need, especially when they are contacting you about their health.
Performance Metrics That Actually Matter
Once your medical call center is up and running, how do you know if it's truly successful? It's about more than just how many calls are answered. Measuring success means looking at metrics that reflect patient trust and improved health, moving far beyond basic numbers like call duration.
Think of it like a health check-up. A doctor doesn't just take your temperature; they look at a range of indicators to get a complete picture of your health. Similarly, a healthy call center is measured by its impact on the patient experience.
Indicators of Quality and Patient Trust
Focusing on the right Key Performance Indicators (KPIs) reveals the real story of your center's effectiveness. One of the most critical is First-Call Resolution (FCR). This metric tracks the percentage of patient issues that are completely resolved in a single interaction, without needing a follow-up call or transfer. A high FCR, ideally over 80%, is a clear sign that your agents are knowledgeable and empowered, which directly reduces patient frustration.
Of course, solving a problem is only half the battle. How did the patient feel during the interaction? This is where Patient Satisfaction (PSAT) comes in. Usually measured with brief post-call surveys, PSAT scores give you direct feedback on agent empathy, clarity, and professionalism. High satisfaction scores are strongly linked to patient loyalty and a positive public reputation for the healthcare practice.
Finally, the most powerful metrics connect call center activities to tangible health outcomes. This is often tracked through clinical adherence, which measures if patients follow through on medical advice after a call. For example, did a patient who called to reschedule actually attend their new appointment? This directly ties the call center’s work to the core mission of healthcare.
Creating an Actionable Dashboard
This data becomes most useful when organized into a performance dashboard. This isn't just a spreadsheet of raw numbers; it’s a tool that helps leaders see trends, pinpoint areas for agent training, and ensure that operational goals support the primary mission of excellent patient care.
Below is an example of what a well-rounded dashboard for a medical call center might include.
Medical Call Center Performance Metrics Dashboard
Key performance indicators for medical call centers with target ranges and measurement methods
| Metric | Target Range | Measurement Method | Business Impact |
|---|---|---|---|
| First-Call Resolution (FCR) | >80% | CRM Data & Post-Call Surveys | Minimizes repeat calls, which reduces patient frustration and operational costs. |
| Patient Satisfaction (PSAT) | >90% | Post-call Surveys (Email, SMS, IVR) | Drives patient loyalty, improves the provider's reputation, and supports patient retention. |
| Appointment Adherence | >95% | EHR/EMR System Tracking | Directly improves health outcomes and secures practice revenue by reducing no-shows. |
| Average Handle Time (AHT) | < 5 minutes | Call Management System Data | Balances agent efficiency with the need for a thorough, un-rushed patient interaction. |
As the dashboard shows, the best metrics create a clear link between call center actions and patient outcomes. It’s about finding the right balance between efficiency and empathy.
By adopting this balanced view, you can evaluate your medical call center not just on its speed, but on its meaningful contribution to delivering better, more compassionate healthcare.
Implementation Strategies That Actually Work

Getting a medical call center running involves much more than just plugging in new phones and installing software. The most successful healthcare practices approach this like they’re opening a new clinical wing—with careful planning, buy-in from key people, and a constant focus on patient safety. A well-thought-out strategy is what separates a high-performing call center from a source of frustration.
A Phased Approach to Success
Jumping in all at once is a recipe for chaos. A measured, step-by-step rollout helps you meet your goals without overwhelming your team. The process should always start with a thorough needs assessment. This means taking a hard look at your practice’s specific communication gaps and understanding what your patients truly require.
These initial findings will shape your technology choices. It's critical that any new system integrates perfectly with your current Electronic Health Record (EHR) and practice management software. A clunky integration creates disconnected data and headaches for your staff.
Of course, technology is only half the picture. Preparing your people for the change is just as important for a smooth transition.
- Build realistic training programs that teach staff how to handle real patient scenarios, not just how to navigate the software.
- Set up clear quality assurance protocols from day one to maintain high standards and track performance.
- Manage the change effectively by clearly showing your team how the new system helps them and improves the patient experience.
Overcoming Common Hurdles
Many call center projects stumble over entirely preventable issues. A classic mistake is underestimating the amount of training required, which leaves staff feeling unprepared and resistant to the new system. Another major pitfall is failing to properly address HIPAA compliance during setup, opening the door to serious security risks.
The most effective leaders get buy-in from clinical staff and administrators from the very beginning. They set practical expectations for timelines and budgets, knowing that building a great medical call center is a marathon, not a sprint.
By achieving and celebrating small, early wins—like a noticeable drop in patient hold times—they build momentum. This proves the project's value and encourages everyone in the organization to adopt the new way of working for the long term.
AI-Powered Solutions: The Future of Patient Communication
Instead of replacing the human touch in healthcare, artificial intelligence is here to support it. Picture an AI as the most dependable assistant for your medical call center team. This assistant works 24/7, handling routine tasks with perfect accuracy, and never needs a coffee break. This frees your skilled human agents to focus their energy and empathy on the complex patient conversations where a human connection matters most.
How AI Augments Human Agents
Today's AI systems use a technology called Natural Language Processing (NLP), which allows them to understand the nuances of human speech. They can grasp what a patient needs, even if the person is upset or uses informal language to ask for an appointment or a prescription refill.
If a call becomes too complex or requires a clinical decision, the AI doesn't hit a dead end. It intelligently passes the conversation to a human agent, along with a complete summary of the interaction and relevant patient information from the EHR. This teamwork between technology and staff helps ensure every patient gets the right help and provides a practical solution to staffing challenges.
Platforms like Simbie AI present this complex information in a clear, manageable dashboard, making advanced technology simple for any clinic staff to use.
Maintaining Empathy at Scale
The goal here is finding the right balance. By letting AI handle the repetitive paperwork, you empower your staff to concentrate on building patient relationships. In fact, clinics that adopt this approach can see administrative tasks reduced by up to 60%, freeing up an incredible amount of time for genuine care.
AI can also provide agents with helpful information during a call, allowing them to offer more personalized and effective support. In essence, these systems function as a highly capable virtual medical receptionist. They offer a dependable first point of contact that makes the patient experience better from the very start and guarantees no call is ever missed.
Your Action Plan for Medical Call Center Success
Knowing what a modern medical call center can do is one thing; putting that knowledge into practice is another. To get real results, you need a clear plan of action. Whether you're setting up your first call center or looking to improve an existing one, these steps will help you make measurable gains in patient communication and operational flow.
Assess and Define Your Goals
Before you can build a solution, you must first understand the problem. Start with a straightforward look at your current communication weak points. Where do patients get stuck? What administrative duties are bogging down your staff?
To get to the heart of the matter, ask your team these key questions:
- Where do our patients experience the most friction or the longest wait times?
- Which repetitive administrative tasks take up the most staff hours?
- How can we offer better and more reliable support after hours?
Build a Phased Implementation Roadmap
With your goals clearly defined, you can create a realistic timeline that won't disrupt your team's critical work. As you look at different vendors, be sure to ask specific questions about security protocols for HIPAA compliance and how they integrate with your EHR system.
Instead of trying to change everything at once, start with a focused pilot program. This approach allows you to demonstrate clear benefits quickly and helps get your clinical staff on board. From the beginning, set clear metrics for success—like a lower call abandonment rate or better appointment attendance—to measure your progress and make a strong case for expanding the program.
Each part of your plan should target a specific, achievable outcome that both strengthens patient relationships and makes your practice more efficient. This methodical approach creates a solid foundation for excellent healthcare communication. If you want to automate routine calls and free up your staff to focus on patient care, it's time to look at a purpose-built solution.
Ready to see how an AI platform can help? Discover Simbie AI today.

