Think of EMR integration software as the central nervous system for a healthcare practice. It’s the critical link that allows all your different software systems—from the lab and pharmacy to billing and scheduling—to talk to each other and share information with your main Electronic Medical Record (EMR). This seamless communication is no longer a luxury; it’s a necessity for modern, efficient healthcare delivery.
Essentially, it acts like a universal translator, making sure every piece of patient data is understood and correctly filed into the central patient chart. This gets rid of the soul-crushing task of manual data entry and drastically cuts down on costly, preventable errors. For practices looking to scale, improve patient outcomes, and reduce staff burnout, understanding and implementing the right integration strategy is paramount. This guide will walk you through the what, why, and how of EMR integration, providing a clear roadmap for transforming your practice's data flow.
Unifying Patient Data for Better Care

Here’s a simple way to picture it: Imagine a patient's medical story is scattered across a dozen different notebooks, each written in a different language. One has lab results, another has billing codes, and a third has notes from a telehealth call. For a doctor to get the full picture, they’d have to hunt down every notebook and painstakingly translate each one. It’s a slow, frustrating process just begging for mistakes. This scenario, while analog, perfectly mirrors the digital chaos in many clinics today.
This is exactly the headache that EMR integration software is designed to solve.
It works by knocking down the digital walls—what we often call "data silos"—that keep all your different healthcare applications from communicating. Instead of your staff being forced to copy and paste information from one screen to another, integration creates automated, secure highways for that data to flow exactly where it needs to go. This creates a single source of truth, a comprehensive patient record that is always up-to-date and accessible.
The Problem of Fragmented Information
When systems can't talk to each other, practices run into a whole host of daily problems that hurt both their efficiency and the quality of patient care. These information bottlenecks are more than just annoying; they create real risks and operational drag that can stifle growth and compromise patient safety.
Without integration, you're likely dealing with:
- Workflow Inefficiencies: Clinicians and admin staff waste huge amounts of time just logging in and out of different systems, hunting for patient data, or re-typing the same information over and over. This "swivel chair" workflow is a major contributor to administrative bloat and staff dissatisfaction.
- Increased Risk of Errors: Any time a human has to manually transfer data, like typing lab values or medication lists from one system into another, the chance of a clinical error skyrockets. These are the kinds of mistakes that can directly impact patient safety, leading to incorrect diagnoses or medication errors.
- Incomplete Patient View: If a provider can't see the whole story in one place, they're forced to make decisions with incomplete or outdated information. That’s a risky way to practice medicine, potentially missing crucial context from a specialist's report or a recent lab result.
- Delayed Care and Billing: Disconnected systems create friction everywhere. Ordering tests takes longer, referrals get stuck in limbo, and submitting claims becomes a complicated, multi-step mess. This slows down patient care and, ultimately, your revenue cycle.
It's no surprise that solving these issues is a top priority. The global EMR market is expected to be worth $33.41 billion in 2025 and is on track to hit $49.62 billion by 2032. A huge chunk of that growth is driven by hospitals, which hold about 42.1% of the market and are desperate to connect their sprawling departmental systems. You can discover more insights about the EMR market growth on coherentmarketinsights.com.
By creating a single, unified source of truth for each patient, this software is the foundation for true healthcare interoperability. It transforms a collection of disconnected data points into a coherent, actionable patient narrative. This shift from fragmented data to a holistic view is what allows clinics to improve clinical efficiency and deliver safer, more coordinated care.
Let's look at how this plays out in the real world. The table below shows the stark contrast between a typical clinic's workflow before and after getting their systems properly integrated.
Impact of EMR Integration on Daily Healthcare Workflows
| Workflow Area | Before Integration (The Manual Way) | After Integration (The Automated Way) |
|---|---|---|
| Patient Check-in | Staff manually types demographic and insurance info from paper forms into the EMR, often leading to typos. | Patient data from the online portal or kiosk flows directly into the EMR, ready for the visit and verified by the patient. |
| Lab Result Review | A nurse receives a faxed lab report, scans it, and manually enters key values into the patient's chart, a time-consuming and error-prone process. | Lab results arrive electronically and are automatically filed into the correct patient's chart, flagging abnormal values for the provider’s immediate attention. |
| Prescription Refills | A patient calls, the MA writes a note, the provider reviews the chart in the EMR, then calls or faxes the pharmacy, creating multiple touchpoints. | A refill request from the pharmacy or patient portal appears in the provider's inbox with the relevant patient data, ready for one-click approval and documentation. |
| Billing and Coding | The biller pores over the provider's notes, manually assigns CPT/ICD-10 codes, and then re-enters them into the separate billing system. | The provider's documentation in the EMR suggests relevant codes, which are then sent to the billing software automatically after the encounter is closed, ensuring consistency. |
The difference is night and day. Automation doesn't just save a few minutes here and there; it fundamentally changes how work gets done, freeing up your team to focus on what actually matters: the patients. This reclaimed time translates directly into better patient engagement and higher staff morale.
The Technology That Makes It All Work
To really get what EMR integration software does, it helps to peek under the hood at the technologies that make this data flow possible. These are the engines that allow completely different systems to have a meaningful conversation. Don't worry, it's not as complex as it sounds—we can break it down with some simple analogies that clarify the core concepts.
The heart of almost all modern integration is the API, which stands for Application Programming Interface. Think of an API like a waiter at a restaurant. Your app (the diner) needs something specific, like a patient's latest lab results. The API (the waiter) takes that order to the EMR system (the kitchen), fetches exactly what you asked for, and brings it back to your table. You never have to go into the kitchen or understand how it works; you just get the data you need in a structured, predictable way.
APIs provide a secure and standardized way for software to talk to each other, forming the backbone of today's best EMR integration software. They're the essential messengers allowing a billing platform to pull service codes from the EMR or a patient portal to display appointment histories in real-time.
The Languages of Health Data
While APIs act as the messengers, the data itself needs to be structured in a language that every system can read. For decades, the industry's go-to standard has been HL7 (Health Level Seven). You can think of HL7 as the formal, traditional grammar of healthcare data. It sets the rules for how information—like patient admissions (ADT messages), lab orders (ORM messages), and test results (ORU messages)—is formatted and exchanged.
HL7 has been a reliable workhorse for years, but its structure can be rigid and a bit clunky, especially for modern web and mobile apps. This complexity opened the door for a more flexible, developer-friendly standard to emerge, better suited for the demands of a connected, on-the-go healthcare ecosystem.
The real goal here isn’t just connecting systems; it’s about building a truly interconnected healthcare ecosystem. This idea, called interoperability, is the key to better patient outcomes and smoother operations. It ensures that data is not just exchanged, but is also usable and meaningful to the recipient.
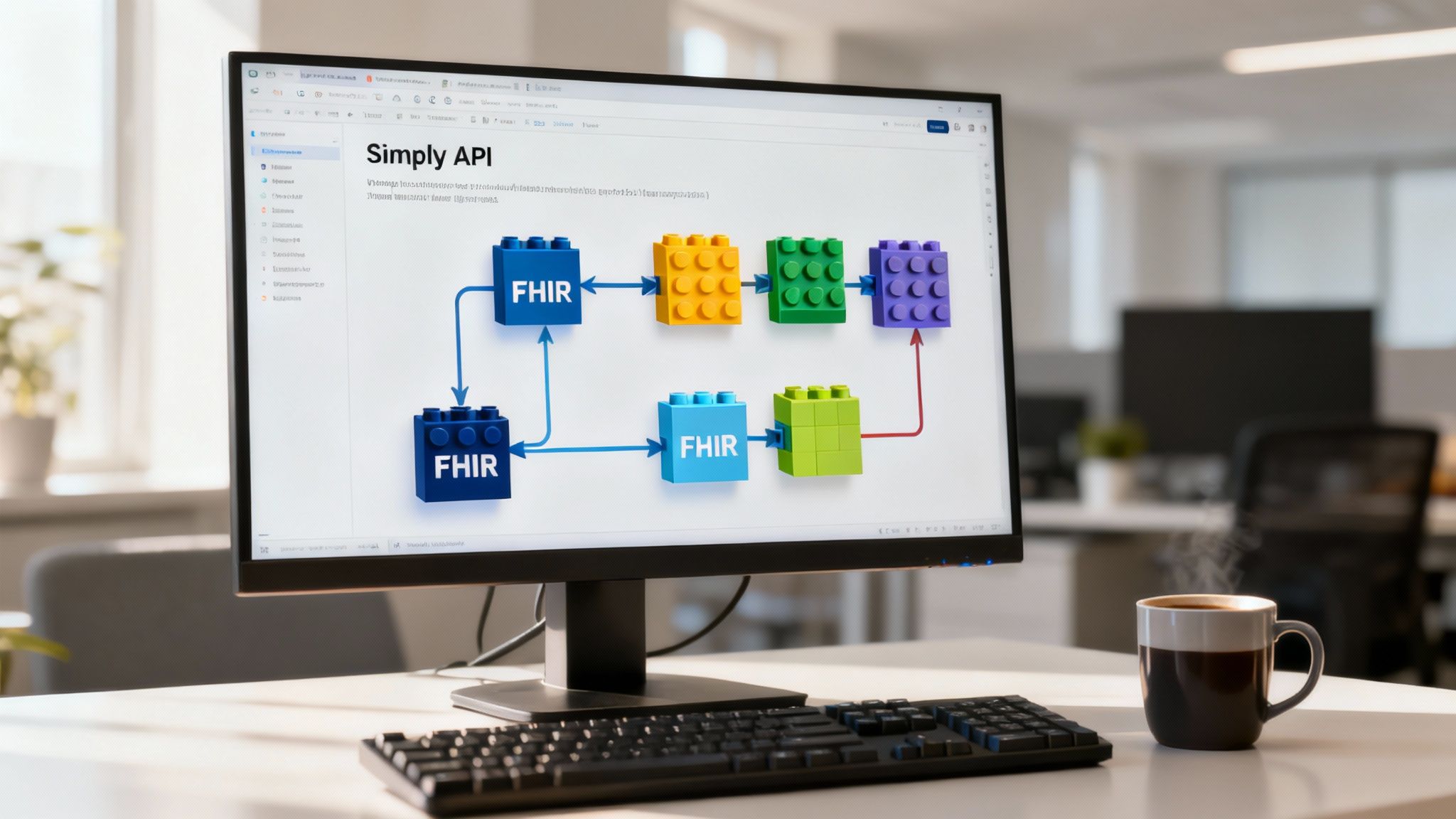
The newer standard is FHIR (Fast Healthcare Interoperability Resources). If HL7 is a strict, old-school grammar book, FHIR is more like a set of digital LEGOs. Each piece of health data—a patient, a medication, an allergy—is a standardized block or "resource." Developers can snap these blocks together quickly and easily to build new applications or connect systems, which is much faster and more intuitive than with older methods. FHIR is built on the same technologies that power websites like Google and Facebook, making it inherently more suited for the internet age.
To dive deeper into this foundational concept, check out our guide on what is interoperability in healthcare.
Comparing the Core Technologies
Knowing the difference between these technologies helps explain why the industry is shifting toward more modern approaches. Each one has a specific job, but they all share the same goal: making data exchange seamless, secure, and reliable.
| Technology | Analogy | Primary Use Case | Key Strength |
|---|---|---|---|
| APIs | A restaurant waiter | The communication bridge between two applications, handling requests and responses. | Enables secure, real-time data requests for modern software and mobile apps. |
| HL7 | A formal grammar rulebook | The traditional standard for messaging between legacy hospital systems (e.g., EMR, LIS, RIS). | Established and widely used for core clinical data like admissions, orders, and results. |
| FHIR | A set of digital LEGOs | The modern standard for building web and mobile health apps and enabling granular data access. | Highly flexible, developer-friendly, and built on modern web standards (RESTful APIs). |
By leveraging these foundational technologies, EMR integration software successfully bridges the gap between systems that would otherwise be isolated. Whether it’s a modern FHIR API connecting a new telehealth app or an HL7 interface talking to a hospital's legacy lab system, these are the tools that break down data silos and create a complete, unified view of the patient.
How Integration Improves Your Practice

It’s one thing to understand the tech, but it’s another thing entirely to see how it solves the daily headaches in your practice. EMR integration isn't just about linking different software together; it's about fundamentally changing how your practice runs. Think of it as turning a collection of disjointed processes into a single, well-oiled machine that operates with greater precision and speed.
This is where the real-world benefits pop up—the kind your staff and patients will notice right away.
Imagine a world where your front desk staff isn't tied up for hours confirming appointments or manually keying in patient information from a clipboard. What if your clinical team received instant alerts for new lab results, right inside the patient’s chart, without ever having to chase down a fax? That’s the reality of a connected healthcare environment, and it is entirely achievable.
The push for EMR integration software is growing for this very reason. While big hospitals made up nearly 60% of the EMR market in 2024, smaller clinics are quickly seeing the light. In fact, a 6.16% annual growth rate is expected for outpatient practices, as more providers look for ways to boost productivity and improve care through smarter data flow. You can read the full research about these EMR market trends.
Erasing Administrative Burdens
One of the first things you’ll notice after integration is how much administrative clutter disappears. Manual data entry is more than just a time-sink; it's a huge source of staff burnout and can lead to some pretty expensive mistakes in both billing and clinical care.
Take a look at how integration transforms these everyday tasks:
- Automated Lab and Imaging Results: Forget having staff manually scan, upload, and attach reports. An integrated system does it for them, automatically filing results into the right patient chart and often flagging abnormal results for provider review. This one change can free up hours every day and gets critical information in front of providers much faster.
- Streamlined Referral Management: Referrals are sent and received electronically, with patient data flowing securely from your EMR to a specialist’s system and back again. No more lost faxes, endless follow-up calls, or delays in getting patients the care they need. This creates a closed loop of communication that benefits everyone.
A fully integrated practice empowers clinicians to spend less time clicking through software and more time actually talking to patients. It shifts the focus from managing data to using data for better decisions, allowing providers to work at the top of their license.
Effective EMR integration is vital for optimizing workflows and patient care within the medical field. Learn more about comprehensive IT services tailored for healthcare practices.
Accelerating the Revenue Cycle
Your practice's financial health is just as important as the clinical care you provide. When your billing systems are disconnected from your clinical workflow, it creates friction that slows down payments and drives up claim denials. EMR integration tackles these financial headaches by building a solid bridge between clinical work and billing.
When a provider finishes an encounter in the EMR, all the key details—diagnoses, procedures, notes—flow straight into the billing software. This automation makes sure claims are accurate, complete, and submitted way faster, significantly improving the health of your revenue cycle management (RCM).
Here’s how that helps your bottom line:
- Reduced Claim Denials: Transferring data automatically from the EMR cuts down on the human coding errors and data mismatches that cause most claim rejections.
- Faster Reimbursements: When claims go out the door right after a visit, you shrink the time between providing a service and getting paid for it, improving your days in accounts receivable.
- Improved Financial Reporting: Integration gives you a clear, real-time snapshot of your practice's financial health, making it easier to spot trends, manage collections, and fix problems early.
Enhancing Patient Care and Safety
At the end of the day, the biggest win from EMR integration is the direct impact on your patients. When a provider can see a complete, up-to-the-minute picture of a patient's health, they can make safer, more confident decisions. A fragmented record is a recipe for disaster, but an integrated one is a tool for excellence.
This single, unified view pulls together data from every single touchpoint—primary care visits, specialist consults, lab results, pharmacy records, even telehealth calls. Having that full story is absolutely critical for making accurate diagnoses, avoiding adverse drug interactions, managing medications safely, and coordinating care that truly improves patient safety and satisfaction. This holistic view is the cornerstone of patient-centered care.
Keeping Patient Data Safe and Compliant
Connecting your healthcare systems is a huge step forward, but it’s only half the battle. The other, arguably more critical half, is making sure every bit of data shared between them is secure and compliant. In healthcare, protecting patient information isn't just good practice—it's the law, mandated by regulations like HIPAA. This is where modern EMR integration software really proves its worth, because it's built with security as a core function, not an afterthought.
Think about it: old-school workflows like faxing paper records are like sending postcards. Anyone along the route could potentially peek at the information. A proper integration strategy replaces those flimsy postcards with armored trucks, creating secure, encrypted, and trackable pathways for data to travel, ensuring end-to-end protection.
Building a Digital Fortress Around Patient Data
There’s a common myth that connecting more systems automatically creates more security risks. When done right, the opposite is actually true. A centralized integration strategy can seriously reduce your practice's vulnerability by replacing scattered, hard-to-track data sharing methods with a controlled, monitored environment where every transaction is logged.
The best EMR integration software provides a multi-layered defense for Protected Health Information (PHI). Two of the most important layers are:
- Data Encryption: This scrambles the data, making it unreadable to anyone without the right key. It’s absolutely essential for protecting information both in transit (as it moves from your lab system to the EMR via an API or HL7 interface) and at rest (when it’s sitting in a database).
- Strict Access Controls: This is all about making sure only authorized staff can see or edit specific patient information based on their role. For example, your billing specialist can access insurance details but shouldn't be able to read sensitive clinical notes. This principle of least privilege is a cornerstone of HIPAA security.
A well-designed integration strategy doesn't just check the box for HIPAA compliance; it creates a fundamentally more secure ecosystem for patient data. It cuts down on the risk of human error and provides a clear, auditable trail of who accessed what information, and when, which is crucial during audits or breach investigations.
This level of security is especially important as EMRs become more specialized. We're seeing huge growth in specialty-specific EMR software for fields like cardiology and oncology, which handle incredibly sensitive patient data. These systems offer tailored tools that improve care, but they absolutely must be integrated with the highest security standards to maintain patient trust and regulatory compliance. You can learn more about specialty EMR trends from this market analysis.
The Critical Role of BAAs and Vendor Trust
When you bring in an integration vendor, you're giving them the keys to your most sensitive data. This is exactly why a Business Associate Agreement (BAA) is non-negotiable. A BAA is a legal contract that holds the vendor to the same strict HIPAA security and privacy standards your practice has to follow. It formally outlines their responsibilities in safeguarding PHI.
Never, ever partner with a software vendor that won’t sign a BAA. That agreement is your assurance that they have the right safeguards in place and will take responsibility for any breach that happens on their watch. When you're evaluating EMR integration software, HIPAA compliance and the vendor's security reputation should be at the very top of your list of vetting criteria.
For practices looking to take the next step with automation, it's crucial to know which solutions are truly built for the healthcare environment. To learn more, check out our guide on finding the right HIPAA-compliant AI tools for your practice.
How To Implement EMR Integration Software
Kicking off an EMR integration project can feel like a massive undertaking, but it doesn't have to be overwhelming. The key is to see it not as a simple software update, but as a fundamental upgrade to your practice's workflow and operational infrastructure. By breaking it down into a clear, step-by-step roadmap, you can make the entire process manageable and set yourself up for a successful, high-impact outcome.
The journey always starts with a good, hard look in the mirror. Before you can find the right solution, you have to truly understand the problems you’re trying to solve and the specific goals you want to achieve.
Phase 1: Assess Your Practice's Unique Needs
First things first, you need to pinpoint the exact workflow bottlenecks that are causing the most friction day-to-day. Where are your staff getting bogged down with manual data entry? Which communication gaps are leading to delays in patient care or creating billing headaches? This is a discovery process that requires input from all stakeholders.
This is the time to get specific. Sit down with your clinical and administrative teams. Ask them what drives them crazy. Map out your current workflows, step by step.
Maybe your nurses are constantly scanning and manually attaching lab results that arrive via fax. Or perhaps your billing team spends hours trying to match telehealth notes with the right claims data because the systems don't sync. Documenting these real-world pain points gives you a concrete shopping list of requirements for your new EMR integration software.
Phase 2: Evaluate Your Current Systems
Next, it's time to take inventory of the technology you already have. When it comes to integration, not all EMRs or third-party apps are built the same. Some modern, cloud-based systems have robust, open APIs that make connecting things relatively straightforward. They are designed for interoperability.
Older, on-premise "legacy" systems, on the other hand, can be a different story. They might have limited capabilities that demand more specialized, custom solutions, often relying on older standards like HL7 v2. Knowing exactly what you’re working with—including software versions and available documentation—is crucial for scoping the project and setting expectations that are actually achievable. This technical audit will be a lifesaver when you start talking to potential vendors.
A successful implementation is built on a solid foundation of self-assessment. Knowing exactly what you need to fix and what tools you're starting with is the key to picking a partner who can truly deliver, rather than one who overpromises and underdelivers.
Phase 3: Choose The Right Integration Partner
Once you have your needs and system capabilities documented, you can start looking for the right partner. This is about so much more than just the tech; it's about finding a team that has real-world healthcare experience and understands the unique challenges of clinical workflows and compliance. As you get started, consulting a comprehensive seamless system integration guide can provide a fantastic primer for what a smooth rollout looks like.
To make an informed decision, you need to ask the right questions and compare vendors apples-to-apples.
Checklist for Choosing Your Integration Partner
Use this checklist to ask the right questions and compare vendors on the criteria that matter most for a successful partnership.
| Evaluation Criteria | Key Question to Ask | Importance (High/Medium/Low) |
|---|---|---|
| HIPAA Compliance & Security | Will you sign a Business Associate Agreement (BAA)? Can you detail your security protocols, data encryption methods, and audit procedures? | High |
| Healthcare Experience | Can you provide case studies or references from practices of a similar size and specialty to ours? Do you understand clinical terminology and workflows? | High |
| Technical Expertise | Do you have direct experience integrating with our specific EMR system and the other applications we use? What standards (HL7, FHIR) do you support? | High |
| Implementation Support | What does your support structure look like during the implementation process? Who is our dedicated point of contact or project manager? | High |
| Post-Launch Support | What happens after go-live? What are your Service Level Agreements (SLAs) for support tickets and system maintenance? Is support 24/7? | Medium |
| Scalability & Future-Proofing | How will your solution grow with us? Can it handle increased patient volume or new services we plan to offer in the future? | Medium |
| Pricing & Transparency | Is the pricing model clear (per-project, subscription, per-transaction)? Are there any hidden fees for implementation, maintenance, or data volume? | High |
Finding a partner who ticks these boxes sets you up for a much smoother journey, not just during implementation but for years to come as your practice evolves.
Phase 4: Plan and Execute The Project
With your partner selected, you'll work together to build a detailed project plan. This roadmap should lay out every single stage, from the initial kickoff meeting to the final go-live date. Think of it as your blueprint, outlining the project scope, setting clear timelines and milestones, and assigning specific roles and responsibilities to people on your team and the vendor’s.
The execution phase is where the technical magic happens—the actual work of connecting the systems, configuring interfaces, and mapping data fields. This is immediately followed by a rigorous testing period. You'll want to run every scenario you can think of, like syncing a new patient registration or transmitting a lab order, to make absolutely sure data is flowing correctly and securely. User Acceptance Testing (UAT) with your own staff is a critical part of this stage.
For a deeper dive into getting the most out of your system after it's connected, check out our guide on electronic health record optimization.
Phase 5: Manage Training and Go-Live
You’re almost there! The final, and arguably most critical, step is preparing your team for the change. You can have the best software in the world, but it’s useless if your staff doesn't know how to use it—or worse, doesn't want to because they are comfortable with the old way.
A thorough training plan is non-negotiable. Your vendor should provide hands-on training that’s tailored to the different roles in your practice. Good change management—clearly communicating the "why" behind the change, highlighting the benefits to their daily work, and supporting your team through the transition—is what will ultimately lead to a smooth go-live and ensure everyone actually uses and embraces the new, more efficient workflows.
The Future of Healthcare Integration

What we’re seeing now with system connectivity is really just the warm-up act. The next chapter in healthcare integration is all about intelligent automation. We’re moving past just swapping data between systems and into a world where AI and voice recognition are completely overhauling how clinicians work, making technology truly ambient and invisible.
The whole point is to finally solve one of medicine's biggest frustrations: the computer screen that sits right between the doctor and the patient, demanding constant attention. It’s about creating a more natural, human way to interact with technology, where the EMR does its job quietly in the background without pulling the doctor's attention away from their patient.
The Rise of Ambient Clinical Intelligence
This next wave has a name: ambient clinical intelligence. Picture this: a system that listens in on the natural conversation between a doctor and patient during an encounter. As they talk, the AI figures out what's clinically important and automatically creates structured notes, suggests relevant diagnoses, and even gets lab orders or prescription refills ready to go in the EMR for the provider's final review.
This is what EMR integration software is evolving into. It's not just about linking two databases anymore; it's about connecting the human conversation directly to the digital record in a meaningful way. The promise here is huge—giving clinicians back their most precious commodity: time. This allows them to focus on the cognitive and empathetic aspects of medicine that machines cannot replicate.
Instead of clinicians spending their days as data-entry clerks for the EMR, intelligent integration makes the EMR work for the clinician. It’s a fundamental shift that gets right to the heart of physician burnout, which is so often driven by a mountain of administrative tasks and "pajama time" spent charting.
The fear that AI will somehow replace doctors just doesn't hold up. The reality is that AI-powered integration will act as a super-capable assistant or "scribe," freeing up doctors to focus completely on treating their patients instead of managing paperwork. This also means fewer manual data entry errors and a clinical record that truly reflects what happened during the visit, not just what the provider had time to type.
Voice AI: The Bridge to Effortless Documentation
Voice recognition is what makes all of this possible. Modern voice AI, like the kind powering platforms such as Simbie AI, does far more than just turn speech into text. It understands clinical nuance, differentiates between speakers (doctor, patient, family member), and can turn a regular, free-flowing conversation into precise, structured medical data that the EMR can understand.
This leap forward means some big changes for the better:
- No More Typing During Visits: Doctors can finally maintain eye contact and build a real connection with patients, knowing the note-taking is handled accurately and comprehensively in the background.
- Reduced Administrative Burden: Those long hours spent after hours catching up on charts? They could become a thing of the past, directly impacting work-life balance and reducing burnout rates across the profession.
- Better Data Accuracy: Because the system captures the details of the encounter as it happens, it's not relying on a provider's memory hours later. This leads to far more complete and accurate records, which improves care quality and billing accuracy.
This isn't some far-off dream. It's the practical and powerful direction healthcare integration is heading. By building intelligence right into the clinical workflow, this next generation of software will finally get the keyboard out of the way of good medicine.
Common Questions About EMR Integration
Even when the benefits are clear, bringing in new technology always raises a few practical questions. For practices looking at EMR integration software, those questions usually boil down to cost, timelines, and how much disruption to expect. Let's tackle some of the most common concerns so you can plan your next steps with confidence.
How Much Does EMR Integration Cost?
This is usually the first question on everyone's mind, and the honest answer is: it really depends. The price tag on an integration project is tied directly to a few key factors, with the complexity of your current setup being the biggest one. The scope of the project is the primary cost driver.
Think of it this way: connecting a modern, cloud-based EMR to a billing platform that's ready to talk to other systems via FHIR APIs is a much simpler—and cheaper—task than trying to integrate an old, on-site legacy system that needs a lot of custom coding and HL7 interface development to play nice.
Other things that will affect the price include:
- The number of systems you’re connecting (labs, pharmacy, scheduling, billing, etc.). Each new endpoint adds complexity.
- The amount and type of data you need to move between them, and whether the data flow is one-way or bidirectional.
- The vendor's pricing structure—are you paying a one-time project fee, an ongoing subscription, or a per-transaction fee?
A simple integration might only cost a few thousand dollars. But for larger practices needing complex, multi-system connections with custom development, the cost can go up substantially. The most important thing is to get a detailed quote that breaks down every possible cost—including implementation, licensing, and ongoing maintenance—before you sign anything.
How Long Does an Implementation Project Take?
Just like cost, the timeline for an EMR integration software project isn't one-size-fits-all. A straightforward integration using modern APIs could be up and running in a few weeks. On the other hand, a more complicated project that involves several legacy systems could easily take a few months from the initial planning session to the final go-live day.
A typical project has several stages: discovery, planning, development, a whole lot of testing, and then staff training. That testing phase is non-negotiable and shouldn't be rushed. It’s where you make sure all the data is flowing correctly and securely before you flip the switch. A good vendor will give you a realistic timeline with clear milestones and keep you in the loop every step of the way.
The best integration projects feel like a true partnership between the practice and the vendor. When everyone is communicating clearly and working toward the same goals, you’re far more likely to stay on schedule and on budget. Open communication and strong project management are key.
What Are the Biggest Challenges to Expect?
While everyone hopes for a perfectly smooth process, it's smart to be ready for a few bumps in the road. One of the most frequent issues is wrestling with older, heavily customized EMRs that just don't want to connect to anything new. These systems often lack modern APIs and can create technical headaches that require some creative problem-solving from your integration partner.
Another major challenge is simply managing the change itself. Getting your staff on board is absolutely critical. If your team isn't trained well or doesn't see the point of the new workflow, they won't use it, and your return on investment will suffer. You have to be proactive about explaining the "why" behind the change—how it makes their jobs easier and improves patient care—and provide fantastic training to make sure the project actually delivers the value you're paying for.
Ready to see how intelligent automation can transform your practice without the implementation headaches? The clinically-trained voice agents at Simbie AI integrate seamlessly with your existing EMR to handle patient intake, scheduling, and refills, freeing your staff to focus on what matters most. Discover how Simbie AI can reduce your administrative overhead by up to 60% and improve patient care at the Simbie AI website.

