At its most basic, an Electronic Health Record (EHR) system is the digital version of a patient’s paper chart. But on its own, it’s just a container. The real magic happens when it starts talking to all the other software you use—a process we call EHR integration.
Think of it like your smartphone. Your calendar, email, and map apps all work together. An email with flight details automatically creates a calendar event, and a tap on the address opens your map app. EHR integrations do the same thing for a healthcare practice, but the stakes are much, much higher.
What Are EHR Integrations, Really?

Without integrations, your staff are stuck in a constant cycle of manual data entry. They're copying and pasting lab results, re-typing billing codes, and shuttling information between different programs. It’s slow, tedious, and a recipe for mistakes.
EHR integration builds digital bridges between these standalone systems. It allows them to share information automatically and securely, turning a static patient file into the dynamic, central hub of your entire practice.
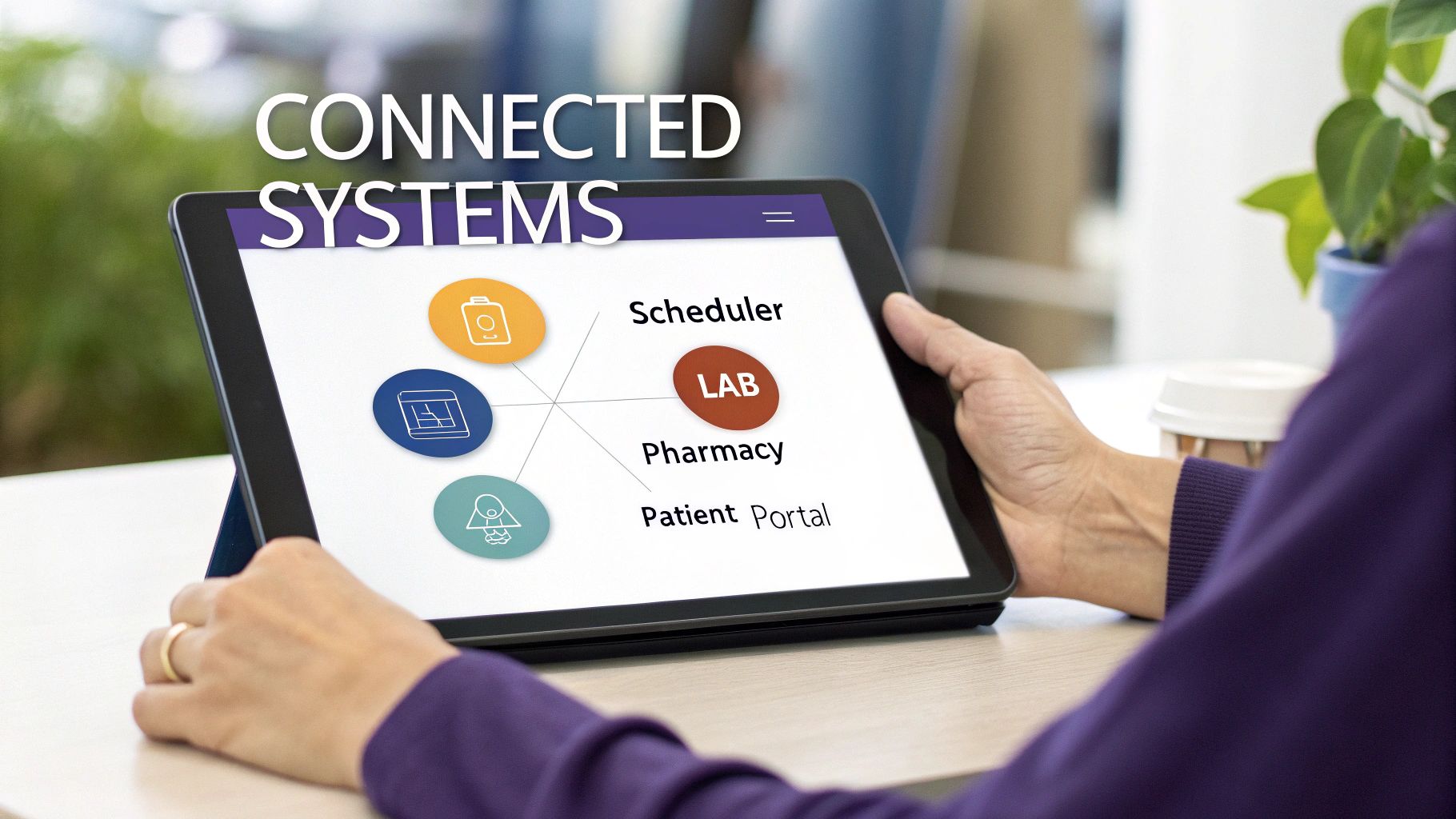
Turning Data Silos into a Connected Ecosystem
In a typical practice, patient data lives in separate, disconnected "silos." Your billing software has one piece of the puzzle, the lab system has another, and the patient portal has yet another. An integration tears down those walls.
It creates a seamless flow of information between all the critical tools you rely on, such as:
- Practice Management Systems (PMS): For handling appointments and billing.
- Laboratory Information Systems (LIS): For sharing test results instantly.
- Patient Portals: For communicating securely with your patients.
- Pharmacy Systems: For e-prescribing and checking medication histories.
When these systems are connected, a lab result can pop up in the patient's chart the second it's ready. A bill gets generated automatically the moment a clinician signs off on their notes. This is the kind of automation that frees up your team to focus on what actually matters: patient care.
The Foundation of Modern Healthcare Operations
This isn't just about making things a little easier; it's a strategic shift in how a practice operates. This free-flowing data is the core of what we call interoperability—the ability for different systems to not just swap data, but to actually understand and use it. To get a better handle on this, check out our guide on what is interoperability in healthcare.
By creating a single, reliable source for all patient information, EHR integrations slash the risk of human error, lighten the administrative load, and give clinicians the complete story of a patient’s health.
Ultimately, a well-integrated EHR turns a simple digital record into an intelligent, active command center for your practice. It’s the technological backbone that supports better clinical decisions, smoother workflows, and safer, more effective care.
What Do EHR Integrations Actually Do For Your Practice?

Connecting your EHR to other software isn't just a technical task—it’s a move that fundamentally changes how your practice works. The benefits ripple out far beyond simple convenience, touching every part of your operation, from the front desk to the exam room. When you break down the walls between your systems, EHR integrations deliver real, measurable improvements for clinicians, staff, and patients.
The numbers tell the story. In 2021, a huge 88% of office-based physicians in the U.S. were already using an EHR, with 78% using a certified system. But just having an EHR isn't enough. The real magic happens when these systems talk to each other. We've seen hospitals get much better at this, with routine health data sharing jumping from 71% in 2018 to 84% in 2023. This trend shows a clear shift toward the kind of connectivity that makes a difference.
Give Your Clinicians a Breather
Think about a typical day for a primary care doctor. A patient comes in with a complicated medical history. Without good integrations, the doctor is forced to play digital detective. They log into a separate lab portal for recent blood work, open another system to find the cardiologist’s notes, and then flip back to the EHR to document the visit. Every click is a distraction.
Now, imagine an integrated system. All that information just flows into the patient's chart. The latest lab results? They pop up automatically. The specialist's notes? They're right there. Suddenly, the physician has a complete picture of the patient’s health in one place. This lets them make smarter decisions, faster, without ever leaving the EHR.
The core idea is simple: a unified view. Stop wasting time hunting for information and give clinicians more time to do what they do best—care for patients.
Make Patient Care Safer and Smarter
A connected EHR is a safer EHR. When your systems can communicate, they create an invisible safety net that catches mistakes before they happen. For instance, when a doctor prescribes a new drug, an integrated system can instantly check it against the patient’s pharmacy records.
If the pharmacy has a note about an allergy that isn't in the EHR, the system can send an immediate alert. This one simple action can prevent a dangerous reaction. It closes the kind of small but critical gaps in a patient's history that can otherwise lead to big problems. This is the foundation for incredible advancements, like those seen in Kaiser Permanente's AI-driven mortality reduction initiatives.
This level of connection powers crucial safety features:
- Automated Drug-Interaction Alerts: Prevents risky medication combos by checking a patient's full history.
- Complete Allergy Information: Pulls data from every source to keep the patient’s record accurate and current.
- Coordinated Care Plans: Ensures specialists, primary care doctors, and other providers are all on the same page.
Lighten the Administrative Load
Let's be honest: administrative work is a huge source of burnout and inefficiency. EHR integrations tackle this head-on by automating the repetitive tasks that bog down your staff, freeing them up for work that actually matters.
Take the average appointment workflow. With integrated systems, you can automate so much of it:
- Appointment Reminders: The scheduler automatically texts or emails patients, which cuts down on no-shows.
- Billing Submissions: As soon as a doctor finalizes their notes, the EHR can send the right codes to the billing software to create a claim—no manual entry needed.
- Payment Posting: Insurance payments are received and automatically posted right in the system.
This kind of automation doesn't just reduce busywork and the risk of costly coding errors. It speeds up your entire revenue cycle. By eliminating these administrative bottlenecks, your practice runs smoother and your team can put their focus back on patients.
Choosing Your EHR Integration Approach

Once you’re sold on the power of a connected healthcare ecosystem, the next big question is: how do you actually build it? There's no one-size-fits-all answer for EHR integrations. The right method really boils down to your practice's size, budget, and where you see yourself in five years.
Let's unpack the common approaches. Think of it like setting up a phone system for your office. If you only need to connect two people, a direct line is simple. But what if you need to connect the entire building? The strategy has to change, and the same goes for your software.
The Direct Line: Point-to-Point Integration
The most straightforward method is Point-to-Point (P2P) integration. This is like running a dedicated, private phone line directly between two systems. For instance, if you need your EHR to talk to your billing software, a developer builds a custom, one-to-one connection just for them.
It's quick and easy for a single link. The problem? This simplicity vanishes the moment you add a third or fourth system. Each new piece of software requires its own dedicated line, quickly creating a tangled "spaghetti architecture" that’s a nightmare to maintain and gets expensive fast.
- Pro: It's a direct, fast connection for one specific purpose.
- Con: It becomes an unmanageable and costly mess as your practice adds more software.
For a tiny practice with just two systems to connect, P2P might seem like a decent starting point. But for almost everyone else, it’s a short-term fix that leads to long-term headaches.
The Switchboard Operator: Hub-and-Spoke Model
A more organized approach is the Hub-and-Spoke model. Picture an old-school telephone switchboard operator—that’s your "hub." Instead of every system having a direct line to every other system, each one just connects to this central hub. The hub then takes care of routing all the messages and data to the right "spoke."
This is a huge step up from the P2P mess. Adding a new system is far easier; you just plug it into the hub instead of building multiple new lines. The whole structure is cleaner and much simpler to manage.
But it has a glaring weakness: a single point of failure. If that central hub goes down, your entire communication network grinds to a halt. All your integrated systems are suddenly cut off from each other. It’s a neat solution, but it puts all your eggs in one basket.
The Universal Adapter: API-Based Integration
By far the most modern and flexible approach is using Application Programming Interfaces (APIs). The best way to think of an API is as a universal adapter. It provides a standardized, secure way for any two pieces of software to plug into each other and communicate, regardless of who made them.
Instead of custom-built lines or a central operator, APIs act like secure, pre-defined doorways. One system can ask for specific information from another, and the API ensures the data is delivered in a format both can understand. This is the bedrock of modern EHR integrations, paving the way for scalable, secure, and adaptable connections.
APIs are the common language of modern software. They let your EHR connect not just to internal systems but also to patient apps, telehealth platforms, and diagnostic tools with surprising ease.
This approach is what’s fueling the massive growth in health tech. The US EHR market hit USD 12.87 billion in 2024 and continues to climb, while the global market is expected to reach $45.9 billion by 2033. This explosion is driven by the urgent need for systems that work together, with 84% of healthcare organizations saying interoperability is critical for better care.
Modern standards like FHIR APIs are at the heart of this movement, making it possible to create plug-and-play connections for everything from patient wearables to AI analytics.
For a deeper dive into the nuts and bolts of connecting these systems, check out our guide on EMR system integration. The API method is truly the way forward, offering the flexibility every growing practice needs.
Comparing Your Integration Options
So, which path is right for you? It’s all about weighing the pros and cons against your specific needs. This table lays it all out to help you make a clear-headed decision.
Comparing EHR Integration Methods
| Integration Method | How It Works | Pros | Cons | Best For |
|---|---|---|---|---|
| Point-to-Point (P2P) | A direct, custom-built connection links two systems. | Simple and fast to set up for a single link. | Gets incredibly complex and expensive to scale; a nightmare to maintain. | Small practices with only two or three systems that need to connect. |
| Hub-and-Spoke | All systems connect to a central integration engine that routes data. | More organized and easier to manage than P2P. | The hub is a single point of failure; if it goes down, everything stops. | Mid-sized practices that need a structured, centralized way to manage data flow. |
| API-Based | Systems communicate using standardized, secure protocols (the APIs). | Highly flexible, scalable, and secure; easily supports modern apps. | Requires your software to have modern, well-documented APIs available. | Any practice that plans for future growth and wants maximum flexibility. |
Ultimately, while P2P might seem tempting for its initial simplicity, an API-based strategy is almost always the smarter long-term investment. It's the only approach that truly prepares your practice for the future of connected healthcare.
Key Systems You Should Integrate with Your EHR
Your EHR shouldn't be a silo. To run a truly modern practice, you need to think of it as the central hub of your entire operation, connecting all the different spokes of your clinical and administrative wheels. The right EHR integrations are all about pinpointing your biggest workflow headaches and connecting the systems that will make a real difference in your day-to-day.
Think of it like building a championship team—every player needs to communicate seamlessly to win. A connected system gets rid of the tedious, soul-crushing cycle of manual data entry, cuts down on human error, and gives your staff precious time back. No more toggling between a dozen different logins or copying and pasting information from one screen to another. Instead, everyone works from a single source of truth.
Practice Management Systems
The absolute must-have integration for any practice is between your EHR and your Practice Management System (PMS). This is the bedrock of your entire operation. Your EHR is the clinical brain—handling notes, charts, and orders—while the PMS is the business brain, managing everything from scheduling and patient demographics to the all-important billing.
When these two systems talk to each other, the payoff is immediate.
- Billing That Just Works: A doctor finalizes a patient visit in the EHR, and the right billing codes are automatically zapped over to the PMS. A claim gets created instantly, without anyone lifting a finger. That's how you speed up your revenue cycle.
- Schedules in Sync: Appointments booked in the PMS pop up right away in the EHR. This gives your clinical team a clear view of their day and ensures patient charts are prepped and ready to go.
- One Patient, One Record: If a patient's insurance or address changes, updating it in one system automatically updates it in the other. This simple sync prevents countless headaches and rejected claims down the line.
Laboratory Information Systems
Few things slow down patient care more than waiting on lab results. Integrating your EHR with a Laboratory Information System (LIS) puts that whole process on autopilot. A clinician can order tests right from the patient's chart, and that's it.
As soon as the results are available, they're sent securely and automatically back into the patient's record. No more staff time wasted downloading, printing, and scanning faxes. More importantly, critical diagnostic data gets to the provider the moment it’s ready, leading to faster, more informed decisions for your patients.
Pharmacy and E-Prescribing Systems
Integrating with pharmacy systems for e-prescribing (eRx) is a non-negotiable for both patient safety and modern convenience. It allows your providers to send prescriptions directly to a patient’s chosen pharmacy right from the EHR. Say goodbye to illegible handwriting and lost paper scripts for good.
This connection is so much more than just a digital fax machine. It’s a powerful safety net. It gives doctors a look at the patient's full medication history and formulary details, helping them spot potential drug interactions and make sure the medication is actually covered by the patient's insurance.
Patient Portals and Engagement Tools
Patients today expect the same digital convenience from their doctor that they get from their bank. A patient portal that’s fully integrated with your EHR is no longer a "nice-to-have"—it's a core requirement for a modern practice. This connection is what empowers patients to get involved in their own healthcare.
An integrated portal lets your patients:
- Check their own lab results and read visit summaries.
- Send in requests for prescription refills.
- Book their next appointment online.
- Message your care team with secure, non-urgent questions.
This doesn't just make for happier patients. It also takes a huge administrative load off your front desk by cutting down on all those routine phone calls. Thoughtful EHR integrations with patient-facing tools are how you build a practice that truly puts the patient first.
How to Navigate Common Integration Challenges
While the benefits of connected systems are obvious, getting there isn't always a straight shot. EHR integration projects can be tricky, but with a bit of planning, the hurdles are completely manageable. It helps to think of them less as roadblocks and more as puzzles to solve.
A successful integration isn't just about plugging in new software. It’s about teaching different systems to have a real conversation. If you get ahead of potential issues, you can build a strategy that tackles them head-on, making the whole process much smoother for your team.
The Data Mapping Dilemma
One of the first puzzles you'll encounter is data mapping. Imagine you're trying to connect two people who speak different dialects. One system might call a patient's birthdate "DOB," while another calls it "Date of Birth." Without a good translator, they're going to misunderstand each other, leading to data errors or lost information.
This little translation problem can pop up everywhere, from insurance details to clinical notes. Even a tiny mismatch can cause big headaches, like a denied insurance claim or an incorrect medication history. The best way to solve this is to invest time upfront creating a detailed "data dictionary" that acts as a universal translator between all your systems.
A solid data mapping strategy isn't just a nice-to-have; it's essential. It makes sure every piece of information keeps its original meaning as it moves from one system to another, which is the bedrock of a trustworthy, integrated network.
Navigating Different Data Standards
Another common challenge is the hodgepodge of data standards floating around in healthcare. For years, different systems used their own languages, like HL7 V2, CDA, or other custom formats. They worked, but getting them to talk to newer technology often required building complex, one-off bridges.
Luckily, the industry is shifting toward a more modern, unified standard: Fast Healthcare Interoperability Resources (FHIR). Think of FHIR as the universal language of modern healthcare data. It uses the same web-based tech that powers many of the apps you use every day, making it far easier for different systems to connect. As you look at new tools, make sure they're built on FHIR—it'll save you a lot of trouble down the road.
Ensuring Bulletproof HIPAA Compliance
Throughout any integration project, HIPAA compliance has to be top of mind. Every time you connect a new system, you're creating another entry point for Protected Health Information (PHI) to be accessed and shared, which naturally increases your security risk. Every single connection has to be secure, encrypted, and monitored.
Here’s a simple checklist to stay on track:
- Conduct a Security Risk Analysis: Look for potential weak spots before you start connecting anything.
- Sign Business Associate Agreements (BAAs): Make sure every vendor you work with is legally on the hook for protecting PHI.
- Implement Access Controls: Ensure staff can only see the specific data they absolutely need to do their jobs. Nothing more.
The world of healthcare tech is moving beyond simple data exchanges. By 2026, EHR integrations are set to become much smarter, using event-driven workflows, FHIR APIs, and AI to finally solve the long-standing problem of fragmented patient data. While smaller practices might still face hurdles in adopting these new tools, new federal rules are pushing to close that gap. You can learn more about the future of healthcare integration and what it means for your practice.
Best Practices for a Successful Integration Strategy
Jumping into an EHR integration project without a clear strategy is like starting a road trip with no map. You’ll definitely end up somewhere, but probably not where you intended to go. A smooth, successful integration is always built on a foundation of careful planning, smart partnerships, and a crystal-clear vision of the exact problems you’re trying to solve.
The very first step—and honestly, the most important one—is to figure out your "why." Before you even think about vendors or technology, you need to be able to state your specific goal. Are you hoping to slash patient check-in times? Speed up your billing cycle? Maybe you need to get rid of those frustrating (and dangerous) errors in lab ordering.
Having a focused objective like this acts as your North Star. It guides every single decision you make from here on out and stops you from sinking money into fancy tech that doesn't actually deliver real value.
Build on a Solid Technical Foundation
Once you know what you want to achieve, it’s time to start looking at the "how"—the right partners and technologies. In today’s interconnected healthcare world, that means making systems built on open standards a top priority.
You’ll want to look for vendors who are all-in on modern protocols, especially Fast Healthcare Interoperability Resources (FHIR). Think of FHIR as a universal translator for health data. It ensures that new tools and systems can connect to your existing setup with way less friction than the clunky, proprietary methods of the past. This approach doesn't just fix today's headaches; it sets your practice up for future innovation and growth.
Don’t just plan for the practice you have today; build for the practice you want to become. Scalability is key. Choose partners and an integration approach, like API-based models, that can grow with you.
Prioritize Security and People
A successful integration isn't just a technical win; it's a human one. You could have the most sophisticated system on the planet, but it's doomed to fail if it isn't secure or if your team doesn't know how to use it properly.
- Implement Robust Security from Day One: Every new connection point is a potential back door for trouble. Make sure you implement strict access controls, run thorough security audits, and get a signed Business Associate Agreement (BAA) from every single partner to keep your practice HIPAA compliant.
- Invest in Comprehensive Training: Technology is only as good as the people using it. Set aside the time and resources for real, hands-on staff training. This is how you drive adoption, make sure everyone is comfortable with the new workflows, and ultimately get the return on investment you're looking for.
Following these practices can turn a daunting project into a manageable one. Of course, the work doesn't stop at go-live. Keeping your systems running at their best is crucial for long-term success. For more on this, check out these practical tips for electronic health record optimization to ensure you’re getting the most out of your technology.
By combining a clear strategy with the right tech and a focus on your team, you can build a connected practice that truly elevates patient care and operational efficiency.
Frequently Asked Questions About EHR Integrations
Even with the best plan in hand, you're bound to have questions as you get into the weeds of an EHR integration. Let's tackle some of the most common ones that pop up.
How Much Does an EHR Integration Project Cost?
There’s no simple price tag, as the cost really depends on how complex your project is. A basic point-to-point connection could be just a few thousand dollars. But if you’re looking at a large-scale integration that connects multiple systems with modern APIs, you could be looking at a range from $25,000 to over $100,000.
What drives that number up or down? A few key things:
- The number of systems you're trying to link together.
- The age and tech stack of your current software (older systems are often harder to work with).
- How much custom work is needed to get data flowing correctly between systems.
- Ongoing maintenance and support fees from your vendors, which you can't forget.
What Is the Difference Between EMR and EHR Integrations?
People often use EMR (Electronic Medical Record) and EHR (Electronic Health Record) interchangeably, but there's a crucial difference that really matters for integration. Think of an EMR as a digital version of a patient's chart within a single practice. An EHR is the big picture—a complete record of a patient's health journey, designed to be shared securely across different providers.
Because of this, EHR integrations are naturally bigger and more focused on interoperability. The goal is to share data with labs, specialists, and hospitals. EMR integrations, on the other hand, are typically more about connecting the systems inside your own practice, like linking your scheduling tool to your billing software.
Why Are Standards Like HL7 and FHIR So Important?
In a nutshell, standards are the common language that allows different healthcare systems to talk to each other without confusion. Without them, every connection would be a custom-coded, one-off project that's a nightmare to maintain.
It's like having a universal translator. Standards make sure that when your system sends patient data, the receiving system understands exactly what it means. This is non-negotiable for patient safety and keeping your practice running smoothly.
HL7 has been the go-to standard for years, but the newer FHIR (Fast Healthcare Interoperability Resources) is now the gold standard. FHIR is built on modern web technologies, which makes it much more flexible and easier for developers to use. It’s the engine powering most new EHR integrations today.
What Should I Look for in an Integration Partner?
Picking the right technology partner is probably the most important decision you'll make in this whole process. You're not just hiring a coder; you're looking for a strategic guide.
Your ideal partner should have a deep and proven track record in healthcare—and with your specific EHR system. They need to be upfront about their process, have rock-solid security to ensure HIPAA compliance, and be there for you with support long after you go live. And here's a big one: make sure they're experts in modern standards like FHIR. That’s a clear sign they’re building for the future, not just patching up yesterday's problems.
Ready to stop administrative overload and give your team the freedom to focus on patients? Simbie AI offers clinically-trained voice agents that seamlessly integrate with your EHR to automate tasks like appointment scheduling, patient intake, and prescription refills. See how our intelligent automation can cut your administrative costs by up to 60%.

