The Dawn of Digital Colleagues: AI in the Clinic
Healthcare is experiencing a significant shift as AI medical staff become powerful collaborators, not replacements. In 2025, these intelligent systems are enhancing capabilities, streamlining workflows, and improving patient outcomes, rapidly becoming indispensable. This listicle explores the key roles of AI medical staff. You will learn about: AI diagnostic assistants, virtual nursing assistants, surgical robots, drug discovery platforms, medical imaging specialists, patient monitoring systems, AI mental health therapists, and AI pharmacists for medication management. Understanding these evolving roles is crucial for modern medical practices integrating advanced technologies for better patient care.
1. AI Diagnostic Assistants
At the forefront of the evolving landscape of AI medical staff, AI Diagnostic Assistants represent a groundbreaking category of tools designed to significantly enhance the accuracy and efficiency of medical diagnoses. These sophisticated systems leverage the power of artificial intelligence, particularly machine learning algorithms, by training on vast, diverse medical datasets encompassing images, lab results, patient histories, and symptom profiles. Their core function is to analyze this complex data, identifying subtle patterns, anomalies, and correlations that might be imperceptible to human observation alone, thereby providing invaluable support to healthcare professionals in the diagnostic process.

The underlying mechanism of these AI assistants, often rooted in deep learning principles pioneered by figures like Geoffrey Hinton, involves training neural networks to recognize indicators of disease. For instance, an AI might be trained on thousands of retinal scans to detect early signs of diabetic retinopathy or on countless chest X-rays to spot nascent lung nodules. By processing this information with remarkable speed and consistency, these systems act as a powerful “second pair of eyes” or an intelligent assistant, augmenting the capabilities of human clinicians. They don’t aim to replace doctors but to empower them, helping to filter noise, prioritize urgent cases, and offer data-driven insights, making them an increasingly indispensable part of modern AI medical staff.
Key Features in Focus:
AI Diagnostic Assistants come equipped with a range of powerful features:
- Advanced Medical Image Analysis: These systems excel at scrutinizing various medical images, including X-rays, CT scans, MRIs, ultrasounds, and digital pathology slides, to detect abnormalities such as tumors, fractures, occlusions, or cellular changes with high precision.
- Pattern Recognition in Comprehensive Diagnostic Data: Beyond images, they can analyze and find correlations in structured and unstructured data like lab results, genetic markers, electronic health records (EHRs), and even patient-reported symptoms to build a more holistic diagnostic picture.
- Real-time Decision Support: Many AI tools integrate directly into clinical workflows, offering immediate analytical feedback and diagnostic suggestions as new patient data becomes available, aiding timely interventions.
- Seamless Integration with Electronic Health Records (EHRs): This allows for efficient data retrieval and input, ensuring that AI-driven insights are readily accessible within the existing patient record system, providing a comprehensive view for clinicians.
- Continuous Learning and Improvement: The most advanced systems are designed to learn from new cases and feedback, continuously refining their algorithms and improving their diagnostic accuracy over time.
The Advantages: Why Embrace AI Diagnostic Assistants? (Pros)
The adoption of AI Diagnostic Assistants offers substantial benefits to healthcare providers and patients:
- Reduces Diagnostic Errors and Misdiagnoses: By providing an objective, data-driven analysis, AI can help catch subtle cues missed by humans, leading to more accurate initial diagnoses and fewer costly, harmful errors.
- Speeds Up Diagnosis Time Significantly: AI can process and analyze medical data far more rapidly than humans, drastically reducing turnaround times for diagnostic reports, which is critical for acute conditions and improving patient throughput.
- Available 24/7 Without Fatigue: Unlike human medical staff, AI systems can operate continuously without breaks or performance degradation due to fatigue, ensuring consistent support around the clock.
- Processes Large Volumes of Data Quickly: AI excels at handling the sheer volume of data generated in modern medicine, from population-level screening to complex individual patient profiles, identifying trends and insights that would be manually unfeasible.
- Identifies Rare Conditions Human Doctors Might Miss: Trained on extensive datasets that include rare diseases, AI can flag conditions that a clinician might encounter infrequently, broadening the diagnostic possibilities.
Understanding the Limitations and Challenges (Cons)
Despite their promise, there are challenges to consider:
- High Initial Implementation Costs: The procurement of AI software, necessary hardware upgrades, integration with existing systems, and staff training can represent a significant upfront investment.
- Requires Extensive and Diverse Training Data: The performance of AI is heavily dependent on the quality, quantity, and diversity of the data it’s trained on. Biased or insufficient data can lead to skewed or inaccurate results.
- Cannot Replace Human Clinical Judgment: AI tools are powerful aids but lack the nuanced understanding, contextual awareness, ethical reasoning, and empathetic communication that human healthcare professionals provide. As Eric Topol, a prominent digital medicine researcher, often emphasizes, the human touch remains paramount.
- May Produce False Positives/Negatives: No AI is perfect. There’s always a risk of incorrect findings, which underscores the need for careful validation and human oversight to confirm AI-generated alerts.
- Regulatory Approval Challenges: Bringing medical AI tools to market requires navigating complex regulatory pathways (e.g., FDA in the U.S., CE marking in Europe), which can be time-consuming and demanding.
Real-World Impact: Notable Examples
Several pioneering organizations and their AI solutions are already making a tangible difference:
- Google’s DeepMind (Google Health team): Notably successful in detecting eye diseases like diabetic retinopathy and age-related macular degeneration from retinal scans, often with accuracy comparable to or exceeding human specialists. Work in this area is heavily influenced by leaders like Demis Hassabis.
- IBM Watson for Oncology (IBM Watson Health division): Designed to help oncologists by analyzing patient data against a vast database of medical literature and clinical trials to suggest potential treatment options.
- Zebra Medical Vision (now part of Nanox.AI): Offers a suite of AI algorithms that analyze medical images to identify a wide array of conditions, assisting radiologists in detecting subtle findings.
- PathAI: Focuses on leveraging AI in pathology to improve the diagnosis of diseases like cancer, aiming to make diagnoses faster and more accurate by analyzing tissue samples.
- Aidoc: Specializes in AI for emergency radiology, automatically flagging acute abnormalities in scans (e.g., brain bleeds, pulmonary embolisms) to help prioritize critical cases.
Strategic Implementation: When and Why to Use This Approach
AI Diagnostic Assistants are particularly beneficial in settings such as high-volume radiology and pathology departments to manage workload and reduce backlogs. They are valuable for large-scale screening programs (e.g., mammography, lung cancer) for early disease detection. Healthcare systems can use them to standardize diagnostic quality and support clinicians in complex or rare disease scenarios. Furthermore, these tools are vital components of an AI medical staff strategy aimed at improving diagnostic speed and precision, ultimately impacting patient outcomes positively, especially in resource-limited environments or telemedicine.
Actionable Tips for Effective Integration
For healthcare practices and systems considering these tools:
- Start with Pilot Programs: Begin by implementing AI diagnostic tools in specific, well-defined areas or departments. This allows for evaluation of their impact, workflow adjustments, and identification of challenges on a smaller scale before wider deployment.
- Ensure Proper Staff Training: Comprehensive training is crucial. Staff must understand not only how to use the AI system but also its capabilities, limitations, and the importance of interpreting its outputs within the broader clinical context.
- Maintain Human Oversight for All AI Recommendations: AI should serve as a decision-support tool. All AI-generated findings or recommendations must be reviewed and validated by qualified healthcare professionals before clinical decisions are made.
- Regularly Validate AI Performance: Continuously monitor and validate the AI’s accuracy against clinical outcomes and established benchmarks. Be prepared to retrain or update models as new data becomes available or an algorithm’s performance drifts.
- Choose Solutions with Strong Regulatory Approval and Data Security: Opt for AI diagnostic systems that have received appropriate regulatory clearances (e.g., FDA approval, CE mark) and adhere to stringent data privacy and security standards (e.g., HIPAA compliance).
2. AI Virtual Nursing Assistants
AI Virtual Nursing Assistants represent a significant advancement in how patient care can be delivered, functioning as intelligent software systems designed to provide round-the-clock support. These sophisticated members of the emerging AI medical staff are not science fiction; they are practical tools revolutionizing patient interaction and management. They offer continuous monitoring, medication reminders, health tracking, and basic medical guidance, directly to patients through accessible digital platforms, effectively extending the reach and capacity of healthcare providers.

At their core, AI Virtual Nursing Assistants leverage cutting-edge technologies like natural language processing (NLP) and machine learning (ML). NLP enables them to understand and respond to patient queries and statements in a conversational manner, whether through text, voice, or even avatar-based interactions. ML algorithms allow these systems to learn from vast datasets of medical information and anonymized patient interactions, continuously improving their accuracy, personalizing their advice, and identifying patterns in patient health data. This data can range from self-reported symptoms to readings from connected health devices. When a situation exceeds their programmed capabilities or a patient’s condition shows signs of serious concern, these virtual assistants are designed to escalate the issue to human healthcare providers, ensuring a seamless safety net and timely intervention.
AI Virtual Nursing Assistants firmly earn their place in any discussion about AI medical staff due to their transformative impact on accessibility, efficiency, and patient engagement. They are not merely ancillary tools but are evolving into integral components of the patient care continuum. By automating routine tasks, providing constant support, and managing large volumes of patient data, they free up human nurses and other clinical staff to focus on more complex, acute, and hands-on patient needs. This redistribution of workload enhances the overall capacity and quality of healthcare services, making them a cornerstone of modern, patient-centric care strategies, particularly in managing chronic conditions, post-discharge follow-up, and promoting preventative health.
Key Features Driving Their Effectiveness:
- Natural Language Conversation Capabilities: Allows patients to interact with the AI in a human-like way, making it easier to report symptoms or ask questions.
- Medication Adherence Monitoring: Goes beyond simple reminders to actively track and encourage compliance, often through interactive check-ins or integration with smart pill dispensers.
- Symptom Tracking and Reporting: Enables patients to log symptoms over time, which the AI can analyze for patterns or concerning trends to share with clinicians.
- Appointment Scheduling and Reminders: Automates the process of booking appointments and sends timely reminders, reducing no-show rates.
- Patient Education and Guidance: Provides patients with reliable information about their conditions, treatments, and self-care practices in an easily digestible format.
- Emergency Situation Detection: Programmed to recognize keywords or symptom combinations that may indicate an emergency, prompting immediate escalation to human responders or emergency services.
Pros: The Advantages for Healthcare Providers and Patients
- Provides Continuous Patient Monitoring: Offers 24/7 vigilance, especially crucial for patients with chronic conditions or those recovering at home, without the constant need for human oversight.
- Reduces Healthcare Costs Significantly: Achieved through automation of routine tasks, reduced hospital readmissions due to better compliance and early intervention, and optimized staff allocation.
- Improves Medication Compliance Rates: Gentle, persistent reminders and educational support can lead to better adherence to treatment plans.
- Accessible to Patients Anytime: Patients can seek information or report concerns at their convenience, improving access to care, especially for those in remote areas or with mobility issues.
- Reduces Workload on Human Nursing Staff: By handling initial queries, routine check-ins, and data collection, these AI assistants alleviate pressure on nurses, allowing them to focus on critical care.
Cons: Navigating the Limitations
- Limited Emotional Connection with Patients: While conversational, AI cannot replicate genuine human empathy, which is vital in many healthcare interactions.
- Cannot Perform Physical Assessments: Diagnosis and treatment often require physical examination, which is beyond the scope of virtual assistants.
- May Struggle with Complex Medical Situations: AI is best suited for common conditions and clear protocols; nuanced or rare cases still require human expertise.
- Privacy and Data Security Concerns: Handling sensitive patient health information necessitates robust security measures and compliance with regulations like HIPAA.
- Technology Adoption Barriers for Elderly Patients: Some patient demographics, particularly older adults, may face challenges with digital literacy or trusting AI-driven healthcare.
Examples of Successful Implementations:
Several companies have pioneered effective AI Virtual Nursing Assistants:
- Babylon Health: Founded by Ali Parsa, this platform offers AI-powered symptom checking, health information, and virtual consultations with doctors.
- Ada Health: Co-founded by Claire Novorol, Ada is a popular symptom assessment app that uses AI to help users understand their health and navigate to appropriate care.
- Sensely: Led by CEO Adam Odessky, Sensely provides virtual nurse avatars that engage patients through empathetic, voice-based conversations for chronic disease management and support.
- Care Angel: This platform focuses on AI-powered chronic care management, using voice interactions to monitor at-risk populations.
- Buoy Health: With CEO Andrew Le at the helm, Buoy offers an AI-driven symptom checker that helps patients understand their symptoms and find the right care options.
When and Why to Implement AI Virtual Nursing Assistants:
This approach is particularly beneficial for:
- Chronic Disease Management: Providing ongoing support, education, and monitoring for patients with conditions like diabetes, hypertension, or COPD.
- Post-Discharge Care: Assisting patients transition from hospital to home, reducing readmission risks through monitoring and adherence support.
- Scaling Routine Patient Communication: Handling frequently asked questions, appointment scheduling, and medication reminders for large patient populations.
- Improving Healthcare Accessibility: Offering initial triage and guidance for individuals in remote locations or with limited access to in-person care.
- Enhancing Patient Engagement: Empowering patients with information and tools to take a more active role in their health management.
Healthcare practices and systems should consider this technology to improve operational efficiency, enhance patient satisfaction, extend care continuity, and allow their human AI medical staff and traditional staff to operate at the top of their licenses.
Actionable Tips for Successful Implementation:
- Implement Gradual Rollout with Patient Feedback: Start with a pilot program in a specific department or with a select patient group. Collect feedback actively to refine the system before a full-scale launch.
- Ensure Clear Escalation Protocols to Human Staff: Define precise triggers and clear pathways for when the AI must transfer the interaction to a human nurse or doctor. This is critical for patient safety.
- Provide Multiple Communication Channels (Voice, Text, Video): Cater to different patient preferences and technological capabilities to maximize adoption and usability.
- Regular Updates Based on Patient Interactions and Medical Advances: The AI system should continuously learn and be updated with the latest medical guidelines and insights gleaned from its interactions.
- Maintain Strict Data Privacy and Security Protocols: Implement robust encryption, access controls, and ensure full compliance with healthcare data regulations (e.g., HIPAA, GDPR) to build patient trust.
AI Virtual Nursing Assistants are more than just a technological novelty; they are becoming an essential element of the modern healthcare landscape, offering tangible benefits for both patients and providers. As this technology continues to evolve, its role within the broader AI medical staff will undoubtedly expand, further shaping a more efficient, accessible, and patient-centered future for healthcare.
3. AI Surgical Robots
The operating room of the future is increasingly populated by sophisticated AI medical staff, and at the forefront of this revolution are AI Surgical Robots. These are not autonomous entities replacing surgeons, but rather advanced robotic systems significantly enhanced with artificial intelligence, designed to assist human surgeons in performing complex procedures with unprecedented precision and control. They function by translating a surgeon’s hand movements into smaller, more precise micro-movements of surgical instruments, often within a minimally invasive context. AI algorithms further augment this by providing real-time data analysis, image guidance, and predictive insights, helping to optimize surgical plans and adapt to unforeseen circumstances during an operation. This synergy between human expertise and robotic capability aims to elevate surgical outcomes, minimize human error, and unlock new surgical techniques previously deemed impossible.
AI surgical robots deserve a prominent place in any discussion about AI in healthcare because they represent a tangible, impactful application of artificial intelligence directly at the point of critical patient care. Their ability to enhance human skill is transforming specialties from urology and gynecology to cardiothoracic and general surgery, making procedures safer and more effective.
Key Features and Patient Benefits:
The capabilities of these AI-enhanced systems are truly remarkable:
- Enhanced Precision and Dexterity: Robotic arms offer a range of motion and stability far exceeding human hands, allowing for meticulous dissection and suturing in confined spaces.
- Real-time Surgical Guidance and Navigation: AI algorithms process live imaging (e.g., from integrated endoscopes) and pre-operative scans to provide surgeons with a detailed, dynamic map of the surgical field. This is akin to a GPS for surgery, guiding instruments with pinpoint accuracy.
- 3D Visualization and Augmented Reality (AR) Integration: Surgeons often operate looking at high-definition 3D displays, offering superior depth perception. AR overlays can project critical information (like tumor boundaries or blood vessel locations) directly onto the surgeon’s view of the patient’s anatomy.
- Tremor Elimination and Motion Scaling: The system filters out natural hand tremors, and surgeons can scale their movements – large hand movements can be translated into micro-movements of the robotic instruments, or vice-versa.
- Predictive Analytics for Surgical Planning: AI can analyze vast datasets of previous surgeries to help predict potential complications or suggest optimal surgical pathways for individual patients before the operation even begins.
- Machine Learning from Surgical Procedures: Many systems are designed to learn from every procedure performed. This collective experience can be used to refine techniques, improve AI assistance, and even identify best practices, continually enhancing the capabilities of the AI medical staff in the OR.
These features translate directly into significant patient benefits, such as reduced blood loss, smaller incisions leading to less pain and scarring, shorter hospital stays, and faster recovery times. The consistency offered by robotic systems also means less variability in surgical outcomes.
The growth and adoption of these sophisticated systems are reshaping the surgical landscape. The following infographic, ‘Surgical Robotics by the Numbers’, visually represents the significant market expansion and current global presence of AI surgical robots, highlighting key data like its projected market value and the number of systems installed globally.
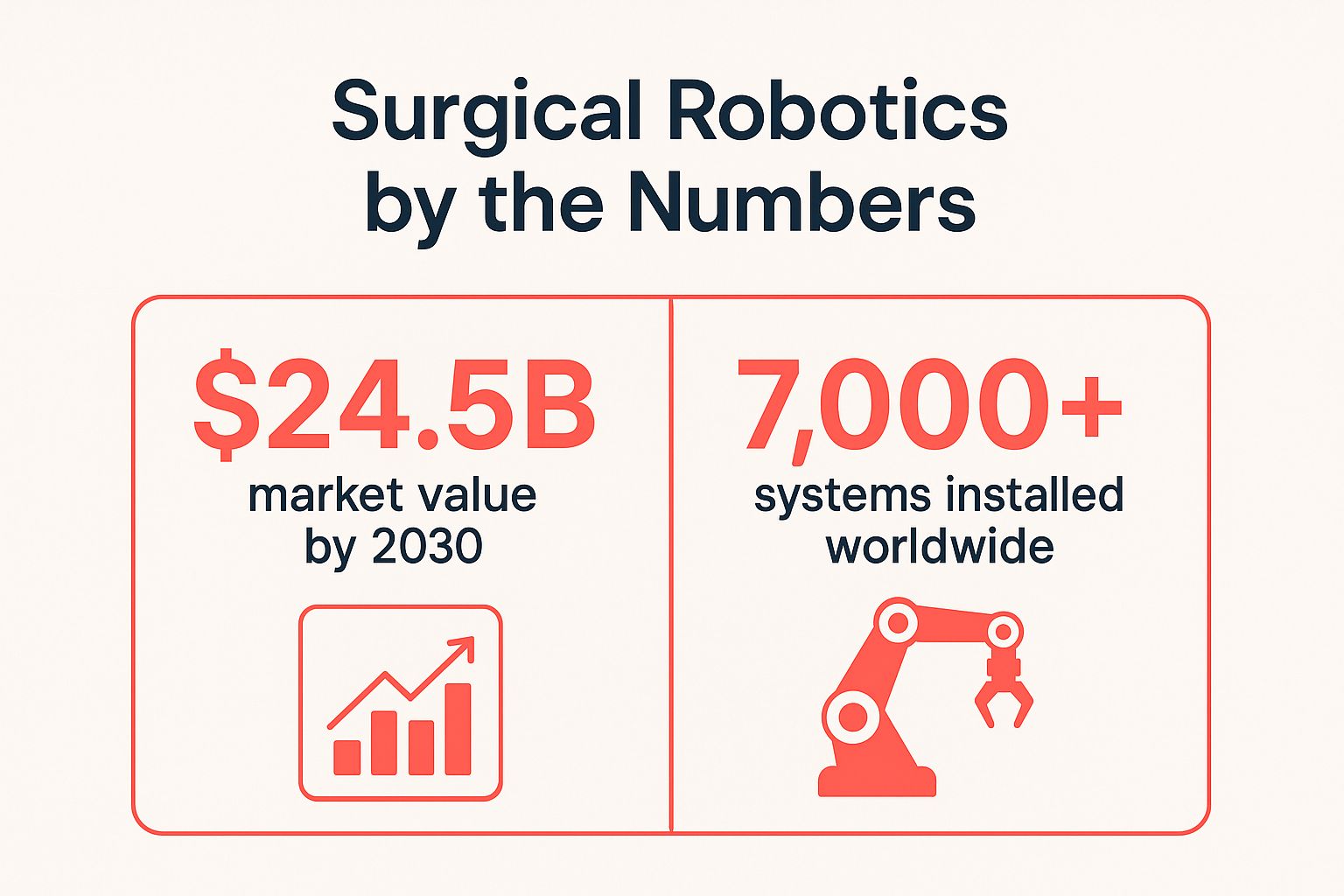
These figures – a projected market value reaching $24.5 billion by 2030 and over 7,000 systems already installed worldwide – clearly illustrate the increasing reliance on and investment in robotic surgery, signaling a transformative shift in surgical care and the growing importance of this segment of AI medical staff.
Weighing the Pros and Cons:
While the advantages are compelling, adopting AI surgical robots involves careful consideration:
- Pros:
- Significantly improved surgical precision and control.
- Reduced patient trauma and faster recovery times due to minimally invasive approaches.
- Consistent performance, as robots do not experience fatigue.
- Enhanced surgical training capabilities through simulators and data analysis.
- Potential to expand the range of patients eligible for complex surgeries.
- Cons:
- Extremely high acquisition and ongoing maintenance costs, posing a barrier for smaller institutions.
- Extensive and specialized training requirements for surgeons and operating room staff.
- Potential for technical malfunctions, though rare, which can interrupt procedures.
- Limited haptic (tactile) feedback for the surgeon compared to traditional surgery, although this is improving.
- Slower adoption rates in some areas due to complexity, cost, and the need for established protocols.
Successful Implementations and Industry Leaders:
Several pioneering companies have brought AI surgical robots into mainstream surgical practice. Intuitive Surgical’s da Vinci Surgical System, co-founded by Dr. Freddie Moll and currently led by CEO Gary Guthart, is perhaps the most well-known, having performed millions of procedures worldwide in various specialties. Other key players include Medtronic’s Mazor X Stealth Edition, specializing in spine surgery; Stryker’s Mako robotic-arm assisted system, widely used for orthopedic joint replacements; CMR Surgical’s Versius system, designed to be versatile and easily integrated into existing ORs, championed by figures like its former CEO Martin Frost; and Johnson & Johnson’s Ottava platform, a newer entrant aiming to offer even greater flexibility. These systems, and the pioneers behind them like Professor Russell Taylor, often hailed as the “father of medical robotics,” exemplify the successful integration of robotics and AI into the modern operating room.
When and Why to Use AI Surgical Robots:
AI surgical robots are most beneficial for complex procedures where precision, minimally invasive techniques, and enhanced visualization are critical. This includes intricate cancer surgeries (e.g., prostatectomies, hysterectomies), delicate cardiac procedures, and complex spinal or neurological operations. Healthcare systems should consider adopting this technology to:
- Improve patient outcomes and safety for specific, high-risk procedures.
- Attract and retain top surgical talent who desire access to cutting-edge tools.
- Offer patients the benefits of minimally invasive surgery, leading to faster recovery and reduced hospital stays.
- Position the institution as a leader in advanced surgical care.
- Ultimately, to provide the best possible care by leveraging the enhanced capabilities these AI-powered tools offer as part of their comprehensive AI medical staff.
Actionable Tips for Adoption:
For healthcare administrators and clinical leaders considering integrating AI surgical robots:
- Invest Heavily in Surgeon Training Programs: Comprehensive, hands-on training and credentialing are paramount for safe and effective use. This includes simulation and proctored cases.
- Start with Less Complex Procedures: Allow surgical teams to build experience and confidence with the system on more straightforward cases before tackling highly complex operations.
- Ensure Robust Technical Support Infrastructure: Reliable, responsive technical support is crucial to minimize downtime and manage any system issues.
- Maintain Traditional Surgical Capabilities as Backup: Robotic systems are tools; traditional skills and equipment must always be available.
- Regular Maintenance and Software Updates are Essential: These systems require diligent upkeep and periodic software upgrades to ensure optimal performance, safety, and access to the latest AI-driven features.
AI surgical robots are more than just machines; they are sophisticated partners in the operating room, augmenting the skills of surgeons and forming a vital part of the growing field of AI medical staff. Their continued development and wider adoption promise to further revolutionize surgical care, making procedures safer, less invasive, and more effective for patients worldwide.
4. AI Drug Discovery Platforms
AI Drug Discovery Platforms are a revolutionary force in pharmaceutical research and development (R&D), acting as highly specialized AI medical staff dedicated to finding new medicines. These sophisticated systems augment human researchers, enabling them to navigate the complexities of drug development with unprecedented speed and efficiency, aiming to drastically shorten the traditional decade-long, multi-billion dollar process. For healthcare systems, administrators, and clinicians, understanding these platforms is crucial as they are poised to deliver the next generation of treatments that will directly impact patient care.
How AI Drug Discovery Platforms Work
These platforms leverage advanced artificial intelligence, particularly machine learning (ML) and deep learning algorithms, to analyze colossal volumes of data. This includes chemical libraries containing millions of molecular structures, vast biological datasets (genomics, proteomics, metabolomics), extensive scientific literature, and historical clinical trial results. The AI then performs critical tasks such as predicting how a molecule will behave in the human body, analyzing its structure to determine potential efficacy, modeling its interaction with specific biological targets (like proteins involved in disease), and even identifying entirely new compounds that might have therapeutic effects. By sifting through complex patterns and relationships at a scale no human team could manage, these digital AI medical staff can pinpoint promising drug candidates significantly faster and more cost-effectively than traditional high-throughput screening or serendipitous discovery methods.
Key Features and Capabilities
The power of AI drug discovery platforms lies in their diverse and interconnected features, each contributing to a more intelligent and streamlined R&D process:
- Molecular Structure Analysis and Prediction: A cornerstone feature, exemplified by systems like DeepMind’s AlphaFold, which can predict the 3D structure of proteins. Understanding protein structure is crucial as most drugs work by interacting with specific proteins.
- Drug-Target Interaction Modeling: AI algorithms simulate and predict how potential drug molecules will bind to specific disease targets (e.g., a rogue protein or enzyme). This helps prioritize candidates most likely to be effective.
- Clinical Trial Optimization: Beyond finding drugs, some AI platforms help design more efficient clinical trials. This includes selecting appropriate patient cohorts, optimizing dosage regimens, and even predicting potential trial outcomes, thereby reducing failure rates and costs.
- Adverse Effect Prediction: Early identification of potential side effects is critical. AI analyzes molecular properties and biological data to predict the likelihood of adverse drug reactions before a drug candidate reaches human trials, significantly improving safety profiles.
- Repurposing Existing Drugs: AI can scan databases of already approved drugs to find new therapeutic uses (indications). This is a faster route to market as these drugs have already passed safety tests.
- Biomarker Identification: These platforms can identify biological markers (biomarkers) that indicate disease presence or progression, or predict a patient’s response to a particular treatment, paving the way for more personalized medicine.
These features collectively allow this advanced form of AI medical staff to refine and accelerate the search for new treatments.
Pros: The Transformative Benefits
The integration of AI into drug discovery offers significant advantages, making it a vital component of the future AI medical staff ecosystem:
- Dramatically Reduced Timelines: AI can condense years of research into months by rapidly screening and prioritizing potential drug candidates.
- Lower Research and Development Costs: By improving efficiency, reducing failures, and optimizing trials, AI significantly cuts down the immense financial burden of bringing new drugs to market.
- Identification of Novel Drug Targets: AI can uncover previously unknown biological targets or mechanisms of disease, opening new avenues for therapeutic intervention.
- Earlier Prediction of Drug Safety: Identifying potential safety issues early in the pipeline prevents costly late-stage failures and, more importantly, protects patient health.
- Enablement of Personalized Medicine: By identifying biomarkers and predicting individual drug responses, AI drug discovery helps tailor treatments to specific patient profiles.
Cons: Challenges and Considerations
Despite their immense potential, AI drug discovery platforms are not without their hurdles:
- Massive Computational Resources: Training sophisticated AI models and processing vast datasets require significant computing power, which can be expensive.
- Dependence on High-Quality Training Data: The performance of these platforms is heavily reliant on the quality, quantity, and diversity of the data they are trained on. Biased or incomplete data can lead to flawed predictions.
- Evolving Regulatory Pathways: Regulatory agencies like the FDA are still developing frameworks for evaluating and approving drugs discovered or designed using AI.
- High Complexity and Specialized Expertise: Developing and interpreting results from these AI systems require multidisciplinary teams of experts, including AI specialists, computational biologists, chemists, and pharmacologists.
- Long Validation Periods Still Necessary: While AI accelerates discovery, identified compounds still need rigorous preclinical and clinical validation, a time-consuming process.
Examples of Successful Implementation
Several pioneering companies and initiatives showcase the real-world impact of AI in drug discovery:
- DeepMind’s AlphaFold: While not a drug discovery platform per se, AlphaFold’s ability to accurately predict protein structures has revolutionized structural biology, providing crucial information for understanding disease mechanisms and designing drugs.
- Atomwise: Employs its AI platform, AtomNet®, for structure-based drug design, screening billions of compounds to identify potential hits for various diseases through numerous collaborations.
- BenevolentAI: Utilizes its comprehensive AI platform to analyze vast biomedical information, aiming to discover novel drug targets and develop new medicines, with candidates progressing through clinical trials.
- Exscientia: A global leader in AI-driven drug design, Exscientia has been the first to advance AI-designed molecules into clinical trials.
- Insilico Medicine: Focuses on applying AI to aging research and drug discovery with an end-to-end AI platform, and has AI-discovered drugs in clinical development.
These examples demonstrate how dedicated AI medical staff in the R&D domain are already making significant contributions.
When and Why to Use AI Drug Discovery Platforms
The adoption of AI drug discovery platforms is becoming increasingly crucial for organizations at the forefront of medical innovation, such as pharmaceutical companies, biotech startups, and academic research institutions. This approach is particularly valuable when:
- Facing the dual challenge of high R&D costs and protracted timelines.
- Seeking to explore novel therapeutic avenues, especially for complex diseases where traditional methods yield diminishing returns.
- Aiming to accelerate the development of personalized medicine tailored to individual patient needs.
Integrating these advanced AI medical staff tools is a strategic imperative for those looking to lead in drug development. For healthcare administrators and clinicians, awareness of these platforms’ capabilities is important, as they will be the source of many future therapies that will transform patient care protocols.
Actionable Tips for Engagement
While direct engagement with AI drug discovery platforms might be specific to research-oriented organizations, the broader healthcare community can benefit from understanding and supporting this evolution:
- For Researchers & Developers:
- Focus on specific therapeutic areas initially to allow for targeted data collection and model refinement.
- Collaborate with academic research institutions to access novel research, diverse datasets, and specialized expertise.
- Ensure access to high-quality, diverse datasets, as this is fundamental for training robust and unbiased AI models.
- Build or secure strong computational infrastructure to handle the demands of AI-driven research.
- Maintain partnerships with pharmaceutical companies to advance discovered compounds through clinical trials and to market.
- For Healthcare Administrators, Clinicians, and Practices:
- Stay informed: Keep abreast of advancements in AI-driven drug discovery as they will shape future treatment options and standards of care.
- Advocate for ethical data sharing: Support initiatives that facilitate secure and ethical data sharing for research purposes, as this data fuels the AI medical staff driving innovation.
- Prepare for personalized medicine: As AI helps develop more targeted therapies, clinical practices will need to adapt to more personalized treatment protocols.
For more detailed information on specific platforms and their work, readers can explore the websites of the example companies mentioned, such as DeepMind (for AlphaFold), Atomwise, BenevolentAI, Exscientia, and Insilico Medicine.
5. AI Medical Imaging Specialists
In the rapidly evolving landscape of healthcare, AI Medical Imaging Specialists are emerging as powerful new members of the “AI medical staff,” transforming how medical images are analyzed and interpreted. These are not general-purpose AI, but highly specialized systems meticulously designed and trained to scrutinize medical imagery with a level of accuracy and speed that can surpass human capabilities. Their core function is to assist human clinicians by providing rapid, consistent, and often remarkably insightful analyses of various imaging modalities, effectively acting as a tireless, highly skilled assistant to human radiologists and pathologists.

How AI Medical Imaging Specialists Work
At their heart, these AI systems leverage deep learning, a sophisticated subset of machine learning, particularly employing architectures known as convolutional neural networks (CNNs). The “intelligence” of these specialists is cultivated through rigorous training on vast, curated datasets, often comprising millions of annotated medical images. This extensive training allows the AI to learn intricate patterns, subtle tell-tale signs of disease, and normal anatomical variations across diverse patient populations. The process involves feeding the AI countless examples of X-rays, CT scans, MRIs, ultrasounds, and even digital pathology slides. Each image in the training set is labeled with specific findings – be it a cancerous tumor, a bone fracture, signs of diabetic retinopathy, or a cardiac abnormality. Through this process, the AI learns to identify these features independently, often detecting nuances that might be imperceptible to the human eye or easily missed during high-volume reading sessions. As an integral part of the modern “AI medical staff,” these specialists continuously learn and refine their algorithms as they are exposed to more data and real-world clinical scenarios, improving their diagnostic prowess over time.
Key Features and Capabilities
AI Medical Imaging Specialists come equipped with a suite of advanced features designed to enhance diagnostic workflows:
- Multi-modal Medical Image Analysis: These systems are often versatile, capable of analyzing images from different modalities. For instance, a single AI platform might be trained to interpret CT scans for lung nodules, MRIs for brain tumors, and X-rays for fractures, offering a comprehensive analytical tool.
- Automated Abnormality Detection: A primary function is to automatically flag suspicious areas or potential abnormalities within an image. This acts as an initial screening, drawing the attention of human radiologists to regions of interest that warrant closer inspection, ensuring critical findings are not overlooked.
- Quantitative Image Analysis: Beyond simple detection, these AI tools can provide precise, objective quantitative measurements. This includes parameters like the size of a lesion, its volume, density, growth rate over time, or blood flow characteristics. Such data is invaluable for tracking disease progression, assessing treatment response, and surgical planning.
- Comparative Analysis Across Time Periods: By digitally aligning and comparing a patient’s current scans with previous ones, the AI can meticulously highlight subtle changes or trends that might be difficult for humans to discern consistently. This is crucial for monitoring chronic conditions or evaluating the effectiveness of ongoing interventions.
- Integration with PACS Systems: Seamless integration with existing Picture Archiving and Communication Systems (PACS) and Radiology Information Systems (RIS) is crucial for practical adoption. This allows AI analyses to be readily available within the radiologist’s existing environment, streamlining workflow without requiring separate, cumbersome software.
- Real-time Image Enhancement: Some AI algorithms can enhance image quality during or immediately after acquisition. This can involve reducing noise, improving contrast, or sharpening details, making it easier for both the AI itself and human eyes to discern critical diagnostic information.
Why AI Medical Imaging Specialists Deserve Their Place: Pros and Cons
The inclusion of AI Medical Imaging Specialists in any forward-thinking “AI medical staff” is driven by their profound potential to revolutionize diagnostic workflows and significantly improve patient outcomes.
Pros:
- Faster Image Interpretation: AI can process and interpret images at a pace significantly faster than human radiologists. This drastically reduces turnaround times for reports, which is critical in emergency settings, for managing large patient volumes, and for expediting treatment decisions.
- Consistent Analysis Without Fatigue: Unlike humans, AI algorithms do not suffer from fatigue, distractions, or inter-observer variability. They provide consistent analysis 24/7, which is especially beneficial during long shifts or for repetitive screening tasks.
- Detection of Subtle Abnormalities: Trained on vast datasets, AI can identify minute or early-stage abnormalities that might be overlooked by human observers, potentially leading to earlier diagnosis when diseases are more treatable.
- Reduces Radiologist Workload: By automating routine screening tasks, prioritizing urgent cases, or providing a reliable “second read,” AI can alleviate the ever-increasing workload on radiologists. This allows human experts to focus their time on more complex cases, interventional procedures, research, and patient consultation.
- Standardizes Interpretation Quality: AI can help standardize the quality of image interpretation across different institutions and among radiologists with varying experience levels, acting as a reliable baseline for diagnostic accuracy.
Cons:
- Cannot Provide Clinical Context: AI typically analyzes images in isolation and lacks the broader clinical context of the patient’s history, symptoms, genetic predispositions, or other test results that a human physician holistically considers.
- May Miss Unusual Presentations: AI models are only as good as the data they are trained on. They may struggle with rare diseases or atypical presentations of common conditions if such examples were not adequately represented in their training dataset.
- Requires High-Quality Image Inputs: The performance of AI is heavily reliant on the quality of the input images. Poor quality scans, artifacts, or non-standardized imaging protocols can lead to inaccurate analyses or failed interpretations.
- Limited Ability to Communicate with Patients: These AI systems are analytical tools; they cannot explain findings to patients, answer their questions, or engage in the empathetic and nuanced communication required in clinical practice.
- Potential for Algorithmic Bias: If the training data used to develop an AI model is not diverse and representative of all demographic groups (age, sex, ethnicity), the AI can inherit and even amplify existing biases, leading to disparities in diagnostic accuracy for certain populations.
Successful Implementations and Examples
The field has seen remarkable progress, with several AI imaging solutions gaining regulatory approval and demonstrating clinical utility:
- Google’s AI for Diabetic Retinopathy Screening: This AI can detect signs of diabetic retinopathy from retinal fundus photographs with an accuracy comparable to human ophthalmologists, enabling wider, more accessible screening programs, especially in underserved areas.
- Mammography AI (e.g., by Hologic, Google Health, Kheiron Medical): Numerous AI algorithms are being deployed to improve the accuracy and efficiency of breast cancer screening by detecting suspicious lesions on mammograms, often acting as a concurrent reader or triaging tool.
- Arterys’ AI for Cardiac MRI Analysis: This FDA-cleared platform uses AI to automate and accelerate the analysis of cardiac MRI scans, providing quantitative data on heart function (like ejection fraction and ventricular volumes) much faster than traditional manual methods.
- Paige.AI for Digital Pathology: Paige focuses on computational pathology, developing AI tools that assist pathologists in detecting cancer and other diseases from digitized microscope slides, improving diagnostic accuracy and efficiency in cancer care.
- Lunit INSIGHT CXR / Behold.ai red dot®: These AIs analyze chest X-rays to detect a range of major lung abnormalities, including nodules, consolidation, and pneumothorax, often acting as a prioritization tool or a second reader for radiologists to enhance detection rates.
When and Why to Use This Approach
AI Medical Imaging Specialists are particularly valuable and should be considered in various clinical scenarios:
- When:
- In high-volume imaging departments struggling with large caseloads and radiologist shortages.
- For large-scale screening programs (e.g., breast, lung, diabetic retinopathy) requiring rapid preliminary reads.
- In resource-limited settings or remote areas where access to specialized radiologists is scarce, AI can provide expert-level assistance.
- For triaging urgent cases in emergency departments by quickly identifying critical findings that require immediate medical attention.
- As a quality assurance tool to provide a consistent second opinion and reduce diagnostic errors.
- Why: The fundamental reason to integrate these tools is their capacity to augment human capabilities. They are a key component of any modern “AI medical staff” aiming to improve efficiency, enhance diagnostic accuracy (especially as a second reader or for detecting subtle findings), reduce turnaround times, standardize care, and ultimately contribute to better patient outcomes by enabling earlier and more precise diagnoses.
Actionable Tips for Implementation
For healthcare practices, clinics, and hospital systems looking to integrate AI Medical Imaging Specialists into their operations:
- Ensure Diverse Training Datasets and Validate Locally: When selecting an AI solution, critically evaluate the diversity of the data it was trained on to mitigate potential biases. Furthermore, conduct local validation studies on your own patient population before full-scale deployment to ensure it performs as expected in your specific environment.
- Implement Robust Radiologist Oversight Protocols: AI should augment, not replace, human expertise. Establish clear “human-in-the-loop” workflows where radiologists review, confirm, or overrule AI findings, especially for critical or unexpected diagnoses. The AI serves as an assistant, enhancing the radiologist’s capabilities.
- Commit to Regular Performance Monitoring and Updates: AI models are not static; their performance can drift over time due to changes in imaging equipment, patient populations, or disease prevalence. Continuously monitor their performance in real-world clinical settings, and ensure they are regularly updated and retrained by vendors as needed.
- Prioritize Seamless Integration with Existing Imaging Workflows: Choose AI solutions that integrate smoothly and intuitively with your existing PACS, RIS, and Electronic Medical Record (EMR) systems. Clunky or standalone systems are less likely to be adopted and can disrupt established workflows, reducing efficiency gains.
- Conduct Continuous Validation Against Clinical Outcomes and ROI: Beyond initial validation, regularly track how the AI’s implementation impacts key performance indicators such as actual patient outcomes, diagnostic accuracy rates, report turnaround times, radiologist workload, and return on investment. This data is crucial for justifying continued use and identifying areas for improvement.
The development and integration of AI Medical Imaging Specialists, driven by the vision of pioneers such as Curtis Langlotz (Stanford radiology AI researcher), Bradley Erickson (Mayo Clinic radiology AI), Eliot Siegel (radiology informatics pioneer), and Keith Dreyer (ACR Data Science Institute), mark a significant leap forward in leveraging technology to enhance healthcare delivery. As these sophisticated systems continue to mature and demonstrate their value, they will undoubtedly become even more integral to the daily operations of medical practices worldwide, functioning as indispensable members of the “AI medical staff.”
6. AI Patient Monitoring Systems
AI Patient Monitoring Systems are a transformative part of modern AI medical staff, offering continuous, intelligent patient surveillance. These platforms use artificial intelligence to meticulously track vital signs, analyze complex physiological data, and, crucially, predict potential health deterioration in real-time. By alerting medical staff to critical changes, they enhance patient safety and care quality, especially in high-stakes environments like intensive care units (ICUs) and busy general hospital wards, acting as vigilant digital assistants.
How AI Patient Monitoring Systems Work
These systems function by integrating data from a multitude of sources, including bedside monitors (tracking heart rate, blood pressure, oxygen saturation), wearable sensors (providing continuous biometrics), and Electronic Health Records (EHRs) for contextual patient history. AI algorithms, often powered by machine learning, then analyze this consolidated data stream. They are trained to identify subtle patterns, correlations, and deviations that might be imperceptible to human observers or only become apparent after intermittent manual checks. This allows them to predict the likelihood of adverse events like sepsis, cardiac arrest, or respiratory failure hours, or even days, in advance.
Key features that define their operation include:
- Real-time Vital Sign Monitoring: Constant, automated tracking of key physiological parameters.
- Predictive Health Deterioration Alerts: Algorithms trained on vast datasets learn to recognize precursors to adverse events, issuing early warnings to clinical teams.
- Integration with Wearable Devices: Extends monitoring capabilities beyond traditional hospital settings or to less acute areas within the hospital, facilitating continuous data capture.
- Automated Documentation: Reduces the manual burden on nursing staff by automatically logging vital signs and other relevant data into the EHR.
- Risk Stratification Algorithms: Help clinicians prioritize care by identifying patients at the highest risk of clinical decline based on comprehensive data analysis.
- Early Warning Systems (EWS): Consolidate multiple data points and AI-driven predictions into a single, actionable score or alert, simplifying interpretation for busy clinicians.
This process transforms raw data into intelligent, actionable insights, a core function of effective AI medical staff, enabling a shift from reactive to proactive patient care.
Why AI Patient Monitoring Deserves its Place: Benefits
AI Patient Monitoring Systems are indispensable to the AI medical staff concept because they directly address some of the most pressing challenges in modern healthcare: enhancing patient safety, managing staff workload, and enabling proactive interventions.
The primary benefit is the early detection of patient deterioration. By identifying subtle negative trends often hours before they would become clinically apparent through routine checks, these systems provide a crucial window for timely intervention. This capability significantly reduces preventable deaths, complications, and lengths of stay.
Furthermore, these systems contribute to optimized staff allocation. Instead of relying solely on scheduled checks or being overwhelmed by constant manual monitoring in high-risk areas, healthcare providers receive targeted alerts, allowing them to direct their attention to patients who genuinely need immediate assessment. This not only improves efficiency but also helps mitigate staff burnout. Another key advantage is continuous monitoring without human fatigue; unlike human staff, an AI system doesn’t get tired or distracted, ensuring consistent vigilance 24/7. Finally, the comprehensive data collection and analysis capabilities provide a rich dataset that can be used for clinical research, quality improvement initiatives, and further refinement of predictive algorithms, creating a virtuous cycle of improvement in patient care.
When and Why to Use This Approach
The application of AI Patient Monitoring Systems is particularly impactful in specific healthcare settings where the benefits of continuous, intelligent oversight are most pronounced:
- Intensive Care Units (ICUs): Given the critical nature of patients and the sheer volume of physiological data generated, ICUs are a prime environment. Here, AI acts as an invaluable member of the AI medical staff, augmenting the capabilities of highly skilled critical care teams.
- General Hospital Wards: These systems can help identify patients on general floors who may be subtly deteriorating, preventing unexpected transfers to higher levels of care or “code blue” events, especially valuable with increasing patient acuity and strained nursing ratios.
- Post-operative Care Units: Patients recovering from surgery are at risk of complications. AI monitoring can provide early warnings for issues like infections or hemodynamic instability.
- Remote Patient Monitoring (RPM): Increasingly, these systems are adapted for RPM programs, allowing continuous oversight of patients with chronic conditions in their homes, potentially reducing hospital readmissions and empowering patients in their self-care.
The decision to implement these systems should be driven by a strategic goal to enhance patient safety, support clinical staff by reducing cognitive load and alarm fatigue (when well-implemented), and leverage data for proactive care in high-risk patient populations.
Examples of Successful Implementation
The value of AI Patient Monitoring Systems as AI medical staff is evident in several leading platforms, with development in this area influenced by pioneers like Blackford Middleton (former CTO of Vanderbilt University Medical Center), Stanford AI researcher Daphne Koller, and Suchi Saria (Johns Hopkins, known for early warning systems).
- Philips’ Guardian Early Warning System (EWS) uses wireless biosensors for automated early warning score calculation and alerts clinicians to subtle signs of deterioration.
- GE Healthcare’s Edison Intelligence platform underpins various applications, including those for patient monitoring, leveraging AI for predictive insights in critical care.
- Epic’s Deterioration Index is integrated within its widely used EHR system, using a predictive model to flag individuals at higher risk of clinical decline.
- ExcelMedical’s WAVE Clinical Platform provides real-time surveillance by aggregating data from various medical devices and EHRs, offering clinicians a comprehensive view.
- Etiometry’s KATE surveillance system employs causal AI to interpret ICU patient data, providing risk analytics and highlighting potential trajectories towards instability.
These platforms, and others like them, demonstrate the practical application of AI in augmenting human clinical capabilities and improving patient safety.
Pros and Cons
While AI Patient Monitoring Systems offer transformative potential as part of the AI medical staff, it’s crucial for healthcare organizations to consider both their advantages and disadvantages.
Pros:
- Early Detection of Patient Deterioration: Significantly improves chances of successful intervention and better outcomes.
- Reduces Preventable Deaths and Complications: Proactive alerts lead to timely care.
- Optimizes Staff Allocation & Reduces Workload: Directs attention where it’s most needed.
- Continuous Monitoring Without Human Fatigue: Ensures 24/7 vigilance.
- Comprehensive Data Collection and Analysis: Provides rich datasets for research and quality improvement.
Cons:
- Initial High Rate of False Alarms: Algorithms may need significant tuning, potentially leading to “alert fatigue” if not managed properly.
- Requires Significant Staff Training: Clinicians need thorough training to understand the system, interpret outputs, and integrate it into workflows.
- Privacy Concerns with Continuous Monitoring: Constant data collection raises privacy and data security concerns requiring robust governance.
- Expensive Implementation and Maintenance: Initial investment and ongoing costs can be substantial.
- Potential for Alert Fatigue: Even with optimized systems, an overabundance of alerts can desensitize staff if alert management isn’t prioritized.
Actionable Tips for Implementation
Successfully integrating AI Patient Monitoring Systems into clinical practice requires careful planning and execution to maximize their effectiveness as AI medical staff:
- Start with High-Acuity Units: Begin deployment in areas like ICUs or step-down units to allow for focused learning and refinement before broader rollouts.
- Customize Alert Thresholds: Work closely with clinical teams to fine-tune alert parameters, balancing sensitivity (catching true positives) with specificity (minimizing false positives) to reduce alarm fatigue and ensure clinical relevance.
- Provide Comprehensive Staff Training: Training should cover system operation, interpretation of predictive analytics, appropriate responses to alerts, and integration into clinical workflows. Identify champion users and provide ongoing education.
- Ensure Regular Algorithm Updates Based on Outcomes: AI models are not static. Regularly evaluate them against actual patient outcomes and update or retrain as needed to maintain accuracy and adapt to changing patient populations.
- Ensure Seamless Integration with Existing Systems: The AI monitoring system must integrate smoothly with hospital infrastructure, particularly the EHR, to facilitate data flow, automated documentation, and ensure insights are accessible within the clinician’s primary workflow.
7. AI Mental Health Therapists
As the healthcare landscape increasingly integrates AI medical staff, one of the most transformative and accessible applications is the AI Mental Health Therapist. These AI-powered therapeutic platforms are engineered to deliver immediate mental health support, offering services like cognitive behavioral therapy (CBT), crisis intervention, and psychological assessment. They represent a crucial innovation, designed to augment the capabilities of human therapists and expand access to mental healthcare, making therapy more affordable and readily available for diverse populations.
How AI Mental Health Therapists Work
AI Mental Health Therapists function through a synergistic blend of sophisticated technologies:
- Natural Language Processing (NLP): This enables the AI to understand, interpret, and generate human-like text, facilitating empathetic and meaningful conversations. Users can express their concerns naturally, and the AI responds therapeutically, often mimicking the interactive style of a human therapist.
- Psychological Frameworks: These platforms are grounded in evidence-based therapeutic modalities. Cognitive Behavioral Therapy (CBT) is a common foundation, guiding users to identify and modify negative thought patterns and behaviors through structured exercises. Other approaches like mindfulness techniques or principles from Dialectical Behavior Therapy (DBT) may also be incorporated to address a range of emotional and behavioral issues.
- Machine Learning (ML): ML algorithms allow these systems to personalize the user experience by learning from interactions, adapting interventions based on user responses, and potentially identifying patterns indicative of a user’s escalating distress. This personalization can improve engagement and the relevance of the support offered, and in some systems, trigger specific support protocols if concerning trends are detected.
Key Features and Their Benefits
These AI systems come equipped with a range of features designed to provide comprehensive mental wellness support:
- Natural Language Conversation Therapy: Offers an interactive, conversational space for users to explore feelings and receive therapeutic guidance, available on demand. This feature aims to create a non-judgmental environment for self-expression.
- Mood Tracking and Analysis: Allows users to log moods, activities, and thoughts. The AI then analyzes this data to provide insights into emotional patterns, potential triggers, and correlations, helping users understand their mental state better.
- Cognitive Behavioral Therapy (CBT) Protocols: Delivers structured, evidence-based exercises and modules directly to the user. These are designed to help manage conditions like anxiety, depression, and stress by teaching practical coping skills.
- Crisis Detection and Intervention: Employs algorithms to identify language patterns or specific keywords indicative of acute distress or a mental health crisis (e.g., self-harm ideation). If detected, the system can provide immediate de-escalation resources, connect the user to emergency hotlines, or alert a human supervisor if integrated into a blended care model. This is a critical safety net.
- Personalized Treatment Recommendations: Tailors suggestions for tools, content modules, and therapeutic techniques based on individual user input, stated goals, and progress, thereby enhancing engagement and the potential effectiveness of the intervention.
- Progress Monitoring and Reporting: Enables users to track their therapeutic progress over time through summaries and visualizations. In blended care models, this data can be shared (with explicit user consent) with human therapists to inform and enrich their sessions.
The collective benefits of these features underscore why AI Mental Health Therapists are a pivotal part of the evolving AI medical staff ecosystem, significantly enhancing accessibility, affordability, and continuous care in mental health.
Pros: The Upside of AI-Driven Mental Support
- 24/7 Availability: Provides immediate mental health support at any time of day or night, which is crucial for individuals experiencing acute distress or those with unconventional schedules.
- Reduces Stigma: Offers an anonymous and private avenue for seeking help, appealing to individuals who might avoid traditional therapy due to social concerns, fear of judgment, or privacy worries.
- Cost-Effective Mental Health Care: Generally more affordable than in-person therapy, with some platforms offering free basic services or tiered subscriptions, thus lowering financial barriers to accessing initial support.
- Consistent Therapeutic Approaches: Delivers standardized, evidence-based interventions with fidelity, ensuring a baseline quality and consistency of care that can sometimes vary with human providers.
- Scalable to Reach Underserved Populations: Can be deployed widely and rapidly to reach individuals in remote geographical areas, those with mobility issues, or populations in regions with a shortage of mental health professionals.
Cons: Recognizing the Limitations
- Cannot Replace Human Empathy and Connection: While AI can simulate empathetic responses, it lacks the genuine warmth, nuanced understanding, intuitive insight, and deep relational connection provided by human therapists.
- Limited Ability to Handle Complex Trauma or Severe Conditions: Not suited for severe mental illnesses, complex trauma, personality disorders, or deeply rooted psychological issues that require the sophisticated judgment, adaptive skills, and intensive support of an experienced human clinician.
- Privacy Concerns with Sensitive Mental Health Data: The collection, storage, and processing of highly personal and sensitive mental health information demand exceptionally robust security measures, transparent privacy policies, and user trust.
- May Miss Subtle Emotional Cues: AI can overlook subtle nuances in language, context, or emotional expression that a human clinician might detect and respond to effectively.
- Regulatory and Ethical Considerations: The field requires ongoing development of clear ethical guidelines, regulatory oversight, and universally accepted standards for efficacy, safety, data governance, and scope of practice.
Examples of Successful Implementations
Pioneering platforms demonstrate the practical application and potential of AI in mental health:
- Woebot Health: (woebothealth.com) Founded by clinical research psychologist Dr. Alison Darcy, Woebot focuses on delivering CBT in a friendly, conversational format, helping users learn to manage symptoms of depression and anxiety.
- Wysa: (wysa.com) Co-founded by Jo Aggarwal, Wysa is an AI-powered emotional health chatbot that acts as an “emotionally intelligent” conversational agent, providing a safe space for users to vent, practice mindfulness, and access a library of evidence-based self-help tools.
- Tess by X2AI: Developed by Michiel Rauws and his team, Tess is a psychological AI assistant often integrated into healthcare systems, university counseling services, and employee wellness programs, providing on-demand support and coaching.
- Replika: (replika.com) While often marketed as an AI companion for general conversation, many users find Replika provides valuable emotional support and a non-judgmental space to talk through issues.
- Ginger: (ginger.com) Ginger offers a comprehensive mental health platform that exemplifies a blended care model, combining AI-driven behavioral health coaching and self-guided content with on-demand access to human coaches and licensed therapists and psychiatrists.
The crisis support research and ethical frameworks developed by organizations like the Koko AI team have also been influential in shaping safe and effective AI interventions for individuals in acute distress.
When and Why to Implement AI Mental Health Therapists
For healthcare administrators, practice managers, and clinical staff, integrating AI Mental Health Therapists can be a strategic move:
- To enhance accessibility and extend reach: Offer support to patients who face barriers to traditional care, such as cost, geographical isolation, transportation difficulties, or stigma.
- As an initial support layer or triage tool: AI can provide immediate assessment and support for individuals with mild to moderate symptoms, freeing up human therapists to focus on more complex cases.
- To supplement traditional therapy: AI tools can act as “digital homework” or inter-session support, reinforcing concepts learned in face-to-face therapy and providing continuous engagement.
- In preventative care and population wellness strategies: Offer AI mental health tools as part of broader wellness initiatives within organizations or communities to promote mental resilience and early intervention.
- To reduce waitlists and provide immediate engagement: Offer an immediate touchpoint for individuals on waiting lists for human therapists, providing support and resources while they wait.
Implementing these tools within an AI medical staff framework helps meet the surging demand for mental health services, improve patient engagement and outcomes through consistent support, and make mental healthcare more integrated and proactive.
Actionable Tips for Effective Implementation
For a successful and ethical rollout of AI mental health solutions, healthcare providers should:
- Clearly Communicate Capabilities and Limitations: Ensure users understand that AI is a support tool and not a replacement for human diagnosis or treatment of severe conditions. Set realistic expectations from the outset.
- Implement Robust Crisis Intervention Protocols: Establish clear, well-defined, and tested pathways for escalating users identified as being in crisis to appropriate human support or emergency services. This is a non-negotiable safety feature.
- Prioritize Data Security, Privacy, and Transparency: Choose platforms with strong end-to-end encryption, transparent data usage policies, and compliance with relevant regulations (e.g., HIPAA in the US). Reassure users about how their data is protected and used.
- Consider Human Therapist Oversight and Blended Care Models: For clinical settings, a blended model where AI tools are used under the guidance, supervision, or in conjunction with human therapists often yields the best results and ensures ethical practice.
- Gather User Feedback and Iterate for Continuous Improvement: Regularly solicit feedback from users and clinicians to understand their experience, assess effectiveness, and identify areas for improvement in the AI tool or its deployment strategy.
- Ensure Strong Data Encryption and Anonymization Techniques: Protect sensitive mental health data with state-of-the-art security measures and, where appropriate, utilize data anonymization or de-identification for research and platform improvement.
AI Mental Health Therapists are a vital and rapidly evolving component of the modern AI medical staff. While they have limitations and are not intended to replace human clinicians, their capacity to democratize access to mental health support, provide consistent evidence-based interventions, and support the work of human therapists is undeniable. They pave the way for a more responsive, accessible, and intelligent approach to mental well-being on a global scale.
8. AI Pharmacists and Medication Management
The pharmacy, a cornerstone of patient care, is undergoing a significant transformation with the integration of AI Pharmacists and Medication Management systems. As a vital component of the emerging “AI medical staff,” these intelligent solutions are not designed to replace human pharmacists but to augment their capabilities, ensuring greater medication safety, optimizing therapeutic outcomes, and streamlining complex pharmacy operations. By leveraging vast drug databases, patient-specific information, and sophisticated algorithms, AI in pharmacy aims to minimize human error and enhance the precision of pharmaceutical care.
How It Works: Precision and Efficiency Unleashed
These advanced systems operate through key features designed to enhance every step of the medication process. Automated drug interaction screening is paramount; AI algorithms meticulously cross-reference a patient’s current medications (including over-the-counter drugs and supplements, if documented) against extensive, continuously updated drug databases. This allows them to flag potential adverse interactions, contraindications, and allergic reactions in real-time, often with greater speed and breadth than manual checks.
AI also facilitates personalized dosage recommendations. By analyzing a rich array of patient-specific data—such as age, weight, kidney and liver function, concurrent conditions, and increasingly, pharmacogenomic information (how an individual’s genes affect their response to drugs)—these systems can suggest optimal dosages tailored to each patient, moving beyond one-size-fits-all approaches.
Medication adherence monitoring is another critical function. Non-adherence is a major impediment to effective treatment. AI-powered tools, ranging from smart pill dispensers like those from Hero Health that track usage and send reminders, to sophisticated mobile applications that engage patients and collect adherence data, help improve compliance with prescribed regimens.
For the pharmacy operation itself, inventory management and forecasting become significantly more efficient. AI analyzes historical dispensing patterns, seasonal demands, epidemiological data, and supplier lead times to optimize stock levels. This reduces waste from expired medications, prevents shortages of critical drugs, and lowers inventory holding costs.
Furthermore, these systems offer robust clinical decision support to human pharmacists. When faced with complex polypharmacy cases or unusual patient profiles, AI can provide evidence-based suggestions, highlight potential risks invisible to the naked eye, and offer alternative therapeutic options, complete with supporting literature. Some advanced AI models are also being developed for adverse drug reaction (ADR) prediction, sifting through large population datasets and individual patient data to identify patterns that might indicate a heightened susceptibility to specific side effects, allowing for proactive adjustments to therapy. The backbone of these powerful capabilities is seamless integration with Electronic Health Records (EHRs), providing the AI with the comprehensive, longitudinal patient data needed for its sophisticated analyses, making these systems integral parts of a cohesive “AI medical staff.”
Why AI Pharmacists Deserve Their Place
AI Pharmacists and Medication Management systems are pivotal members of the “AI medical staff” concept, profoundly impacting medication safety and efficacy. Their primary benefit is significantly reducing medication errors—a major patient safety concern—through precise, automated checks of dosages, interactions, and allergies. They optimize drug therapy effectiveness via personalized dosing and diligent interaction screening, ensuring patients receive the most suitable treatment. AI also demonstrably boosts medication adherence rates with smart monitoring and timely reminders, tackling a key cause of treatment failure and increased healthcare costs.
Operationally, AI streamlines pharmacy workflow. By automating repetitive and time-consuming tasks like pill counting, packaging (as seen with PillPack’s innovations), initial screening for interactions, and inventory management, it frees up highly trained pharmacists and technicians. This allows them to dedicate more time to crucial clinical duties, such as direct patient counseling, Medication Therapy Management (MTM), immunizations, and collaborative care with other healthcare providers. This shift not only enhances efficiency and potentially reduces operational costs but also improves job satisfaction for pharmacy staff and supports 24/7 medication oversight in certain capacities.
Examples of Successful Implementation
The practical application of AI in pharmacy is already well-established and growing:
- ScriptPro (scriptpro.com): Offers a suite of robotic pharmacy systems that automate prescription filling and dispensing with remarkable accuracy and speed, particularly beneficial in high-volume community and hospital outpatient pharmacies.
- Omnicell (omnicell.com): A leading provider of automated dispensing cabinets (ADCs) and medication management solutions for hospitals and other healthcare facilities. Their systems help ensure controlled access to medications, accurate tracking, and reduced risk of diversion.
- PillPack (now Amazon Pharmacy) (pharmacy.amazon.com): Co-founded by TJ Parker, PillPack revolutionized medication management for individuals with multiple prescriptions by using automation and AI to sort and package medications into personalized, pre-sorted packets by date and time, delivered to the patient’s home.
- Hero Health (herohealth.com): Founded by Kal Patel, Hero Health focuses on improving in-home medication adherence with its smart medication dispenser that sorts, dispenses, tracks usage, and sends alerts to patients and caregivers.
- Parata Systems (parata.com): (Now part of BD) Provides a range of pharmacy automation solutions, including vial-filling robots and pouch packaging systems, aimed at improving efficiency, safety, and adherence in retail and long-term care pharmacies. Randal Flick was instrumental in ScriptPro’s early innovations.
These companies, alongside the ongoing work of numerous academic pharmacy informatics researchers, vividly demonstrate how “AI medical staff” are successfully enhancing various stages of the medication management lifecycle.
When and Why to Use AI Pharmacists
The adoption of AI pharmacists and medication management systems is particularly advantageous in specific contexts:
- When to Use:
- In high-volume pharmacies (retail, hospital, mail-order) that process thousands of prescriptions daily, to enhance speed, accuracy, and efficiency.
- Within healthcare systems strongly focused on reducing medication errors and improving overall patient safety metrics.
- For managing patients with complex medication regimens, such as the elderly or individuals with multiple chronic conditions (polypharmacy).
- In organizations aiming to improve medication adherence rates across specific patient populations known for lower compliance.
- In practices and health systems looking to free up pharmacist time from dispensing tasks to allow for expansion of clinical services and more direct patient interaction.
- Why to Use:
The fundamental motivations are to enhance patient safety by minimizing preventable medication errors; improve therapeutic outcomes through more personalized and precisely optimized drug therapy; increase operational efficiency, leading to potential cost savings and better resource allocation; support overburdened pharmacy staff by reducing manual workload and mitigating burnout; and to leverage vast amounts of data for better clinical and administrative decision-making. Integrating this sophisticated type of “AI medical staff” ultimately helps create a more responsive, precise, and patient-centered pharmacy service.
Actionable Tips for Implementation
For healthcare organizations—from small practices to large systems—considering the implementation of AI in their pharmacy services, a strategic approach is key for success:
- Implement Comprehensive Staff Training Programs: Ensure all pharmacy staff, from technicians to pharmacists and administrators, are thoroughly trained on how to use the new AI systems. This includes understanding their capabilities, limitations, and how they integrate into (and potentially reshape) existing workflows to foster buy-in and effective utilization.
- Ensure Seamless and Secure EHR Integration: The effectiveness of AI pharmacists heavily relies on access to comprehensive, accurate, and up-to-date patient data. Prioritize systems that can integrate deeply and securely with your existing Electronic Health Record (EHR), Computerized Physician Order Entry (CPOE), and other relevant clinical information systems.
- Commit to Regular Updates to Drug Databases and Algorithms: Drug information is constantly evolving with new medications, updated guidelines, and emerging interaction data. Work with AI vendors who demonstrate a commitment to timely, validated updates to their core drug interaction databases, clinical guidelines, and the AI algorithms themselves.
- Maintain Robust Pharmacist Oversight for Complex Cases: While AI is a powerful tool, it is not infallible and should not replace critical human judgment. Establish clear protocols where human pharmacists review AI-generated recommendations, especially for complex patients, unusual or high-alert interactions, or when the AI flags significant concerns. The “AI medical staff” should support, not supplant, the indispensable expertise of human pharmacists.
- Focus on High-Volume, Routine Medications or Processes Initially: Consider a phased implementation strategy. Start by automating or applying AI to the management of high-volume, routine prescriptions or specific error-prone processes. This allows the organization to gain experience, demonstrate value, identify and resolve integration challenges, and refine processes before expanding to more complex areas or full-scale deployment.
Challenges and Considerations (Cons)
Despite the compelling benefits, organizations must be aware of and plan for potential challenges:
- Cannot Provide Hands-On Patient Counseling: AI lacks the empathy, nuanced communication skills, active listening, and ability to read non-verbal cues that are essential for effective, compassionate patient counseling—a critical role that remains firmly in the domain of human pharmacists.
- Limited Understanding of Subjective Patient Preferences: AI typically doesn’t account for individual patient lifestyle choices, cultural beliefs, socio-economic factors, or personal preferences regarding medication formulations or schedules, unless this data is specifically captured and the AI is programmed to consider it.
- Requires Complex Integration with Multiple Systems: Achieving true interoperability can be a significant hurdle. AI pharmacy systems need to seamlessly and securely connect with disparate systems like EHRs, laboratory information systems, billing systems, and inventory systems, which can be technically complex, time-consuming, and costly.
- May Miss Complex or Atypical Clinical Contexts: While AI can process vast amounts of data, it may not always grasp the full, holistic clinical picture or subtle, atypical nuances that an experienced clinician would recognize through intuition and broader contextual understanding. Over-reliance without critical human oversight can lead to errors of omission or commission.
- Regulatory Compliance and Transparency Challenges: Ensuring that AI algorithms are validated, auditable, free from bias, and comply with healthcare regulations (like HIPAA for data privacy in the US, GDPR in Europe) is an ongoing and evolving concern. The “black box” nature of some complex AI models can make transparency, explainability, and accountability difficult to achieve, posing challenges for regulatory approval and clinical trust.
AI Medical Staff: Key Feature Comparison
| Concept | Implementation Complexity 🔄 | Resource Requirements ⚡ | Expected Outcomes 📊 | Ideal Use Cases 💡 | Key Advantages ⭐ |
|---|---|---|---|---|---|
| AI Diagnostic Assistants | High: Requires extensive training data, regulatory approval, integration with health records | High: Needs large datasets, computing power, clinical validation | Improved diagnostic accuracy, reduced errors, faster decisions | Disease diagnosis, radiology, pathology | Reduces misdiagnoses, identifies rare conditions, 24/7 support |
| AI Virtual Nursing Assistants | Moderate: NLP integration, escalation protocols, privacy compliance | Moderate: Cloud-based, patient data handling, multi-channel communication | Continuous patient monitoring, medication adherence, cost savings | Patient care support, medication reminders, health education | Reduces nurse workload, accessible anytime, improves compliance |
| AI Surgical Robots | Very High: Expensive hardware, surgeon training, maintenance | Very High: Robotics infrastructure, ongoing technical support | Enhanced surgical precision, reduced recovery times | Minimally invasive surgeries, complex procedures | Tremor elimination, augmented reality, consistent performance |
| AI Drug Discovery Platforms | Very High: Requires specialized expertise, vast computational resources | Very High: HPC clusters, deep datasets, interdisciplinary teams | Faster drug discovery, cost reduction, novel therapeutics | Pharma R&D, molecular analysis, clinical trial optimization | Accelerates timelines, predicts safety, enables personalized meds |
| AI Medical Imaging Specialists | High: Needs diverse image datasets, PACS integration, radiologist oversight | High: Large annotated imaging databases, real-time processing power | Faster, consistent image analysis, abnormality detection | Radiology, pathology, multi-modal imaging | Reduces workload, detects subtle anomalies, standardizes quality |
| AI Patient Monitoring Systems | High: Sensor integration, real-time alert customization, staff training | High: Continuous data streaming, alert systems, hospital IT infrastructure | Early deterioration detection, reduced mortality | ICUs, hospital wards, real-time vital monitoring | Prevents avoidable deaths, optimizes staff use, continuous data |
| AI Mental Health Therapists | Moderate: NLP with psychological frameworks, crisis protocols | Moderate: Secure data handling, continuous updates | Increased access to therapy, reduced stigma, cost-effective care | Mental health support, CBT delivery, crisis intervention | 24/7 availability, scalable, consistent therapy approaches |
| AI Pharmacists & Medication Management | Moderate: Integration with EHRs, drug databases, clinical decision support | Moderate: Automated dispensing, monitoring systems | Fewer medication errors, improved adherence, workflow efficiency | Pharmacy operations, medication safety, dosage optimization | 24/7 medication guidance, error reduction, optimized therapy |
Embracing Your New AI Teammates: The Path Forward
The journey through the landscape of AI medical staff reveals a transformative horizon for healthcare. As we’ve explored, the applications are diverse and impactful, ranging from AI diagnostic assistants sharpening clinical accuracy and AI virtual nursing assistants providing round-the-clock support, to AI surgical robots enhancing precision, AI drug discovery platforms accelerating innovation, and AI medical imaging specialists offering deeper insights. The integration of AI patient monitoring systems, AI mental health therapists, and AI pharmacists further underscores the comprehensive support these new digital colleagues provide. The most crucial takeaway is that the rise of AI medical staff signifies a monumental shift towards more efficient, accurate, and accessible healthcare for everyone.
Platforms like Simbie AI are at the forefront of this evolution, particularly in streamlining the often-overwhelming administrative tasks. By deploying clinically-trained voice agents to manage patient intake, appointment scheduling, and prescription refills, they exemplify how targeted AI solutions can free human staff to dedicate their invaluable expertise to direct patient care and complex clinical decision-making. Embracing these innovations thoughtfully is no longer a futuristic ideal but a present-day necessity for practices aiming to thrive in 2025 and beyond.
So, what are the actionable next steps for healthcare providers and administrators?
- Assess Your Needs: Identify specific areas within your practice—be it administrative overload, diagnostic support, or patient communication—where AI medical staff could offer the most significant improvements.
- Educate and Collaborate: Foster an environment of learning and collaboration. Equip your human team with the knowledge and skills to work alongside their new AI teammates effectively.
- Start Strategically: Consider pilot programs for specific AI tools. This allows for gradual integration, learning, and adjustment, ensuring a smoother transition.
- Prioritize Data Security and Ethics: As you explore AI medical staff solutions, ensure they meet stringent data privacy and ethical guidelines to maintain patient trust.
Mastering the integration of AI medical staff is invaluable because it unlocks a cascade of benefits: enhanced diagnostic speed and accuracy, reduced workload and burnout for human staff, optimized operational workflows, and ultimately, improved patient outcomes and satisfaction. This isn’t just about adopting new technology; it’s about fundamentally redesigning healthcare delivery to be more proactive, personalized, and patient-centric. The broader impact is a healthcare system better equipped to meet the challenges of today and the opportunities of tomorrow.
The path forward involves a synergistic partnership between human ingenuity and artificial intelligence. By embracing AI medical staff not as replacements, but as powerful allies, we can collectively build a healthier future, where technology empowers medical professionals to deliver the best possible care.
Ready to empower your practice with the administrative capabilities of AI medical staff? Discover how Simbie AI’s clinically-trained voice agents can automate routine tasks like patient intake and scheduling, freeing your team to focus on critical patient care. Visit Simbie AI to learn more and see how they can become an invaluable part of your team.

