Why Long Wait Times Are Killing Your Practice

Let's be frank, waiting rooms aren't fun. And in healthcare, a long wait is more than just annoying—it can genuinely hurt your practice. I've chatted with so many healthcare administrators and staff who've seen this firsthand. The ripple effect of long wait times is real, impacting everything from patient satisfaction and staff morale to, yes, your bottom line.
One of the most immediate impacts? Patient trust takes a hit. When patients consistently wait well past their appointment time, they feel like their time isn't valued. This can spiral into negative reviews, patients leaving, and a general sense of frustration. Think about it: if you were constantly kept waiting, wouldn't you start questioning the practice's respect for your time, and ultimately, their commitment to your care?
It also hits you where it hurts: revenue. Longer wait times often mean more no-shows. If a patient expects a long wait, they're much more likely to cancel or just not bother showing up. Empty appointment slots equal lost revenue. Plus, inefficient scheduling due to these delays limits the number of patients you see each day, impacting your earning potential even more.
And then there's the staff burnout. Healthcare professionals are already under so much pressure. Constantly running behind only adds to the stress. This leads to lower job satisfaction, higher turnover, and even a decline in the quality of care. It’s a downward spiral. The impact of wait times on actual health outcomes is significant. Delays can lead to worsening conditions, and even hospitalizations. The Philips Future Health Index 2025 report found that 33% of patients saw their health worsen due to delays, and over 25% ended up in the hospital because of long wait times. Check out the Philips Future Health Index 2025 report for more on this.
The Real Cost of Waiting
Addressing long wait times isn't just about improving patient flow. It’s about building a sustainable, successful practice. Understanding the true cost of these delays lets you make a strong case for change and find solutions that help everyone: your patients, your staff, and your practice.
Let's look at how wait times stack up around the world to give you some context. The table below shows a snapshot of average wait times for different types of appointments and tests.
Global Healthcare Wait Time Comparison
Comparative analysis of average wait times across different countries and healthcare systems
| Country | GP Appointment Wait | Specialist Appointment Wait | Diagnostic Test Wait |
|---|---|---|---|
| Canada | 4 weeks | 10 weeks | 8 weeks |
| United States | 2 weeks | 6 weeks | 4 weeks |
| United Kingdom | 2 weeks | 8 weeks | 6 weeks |
| Germany | 1 week | 4 weeks | 2 weeks |
| France | 1 week | 3 weeks | 2 weeks |
As you can see, wait times vary quite a bit. While some countries manage to keep waits relatively short, others face significant delays. This underscores the importance of optimizing your processes to stay competitive and provide timely care.
In the next sections, we’ll explore actionable strategies for reducing patient wait time and building a better experience for everyone involved.
Tracking What Really Drives Patient Frustration

Forget simply clocking wait times. That’s addressing the symptom, not the disease. Truly reducing patient wait time means understanding the root of patient frustration. I've seen this firsthand working with high-performing clinics that use data to dig deeper.
For example, one clinic discovered patients weren't bothered by the length of the wait, but the uncertainty. They felt abandoned, clueless about the wait time or the reason for the delay. The solution? Digital displays in the waiting room showing estimated wait times. Patient satisfaction shot up, even without changing actual wait times.
Communication is also huge. A quick, friendly explanation for a delay works wonders. Another clinic implemented nurse check-ins with waiting patients, acknowledging the delay and giving a realistic timeframe. This drastically reduced frustration. And this is important because reducing patient wait times is a global struggle. The average appointment wait time is currently 31 days, a 19% increase since 2022. For a deeper dive into these trends, check out Deloitte's 2025 Global Health Care Executive Outlook.
Key Metrics Beyond the Clock
Traditional metrics like average wait time are necessary, but they’re just one piece of the puzzle. Here are other key performance indicators (KPIs) that truly reflect the patient experience:
- Perceived Wait Time: How long the patient feels they're waiting. Patient surveys and feedback forms are great for this.
- Wait Time Variability: Inconsistent wait times are more frustrating than consistently long waits. Track the range and standard deviation.
- Patient Sentiment: Analyze patient reviews and feedback for wait-time-related keywords and overall satisfaction.
- No-Show Rates: High no-shows can subtly signal patient frustration with long waits.
Early Warning Signs
Catching bottlenecks early is critical. Look for patterns, like consistently long waits for certain appointment types or providers. Simbie AI's process improvement resources might give you some ideas on optimizing your workflow. This proactive approach lets you tackle problems before they snowball into bigger issues. By focusing on these metrics, you'll not only reduce wait times but also improve the entire patient experience.
Transforming Your Daily Operations For Better Flow
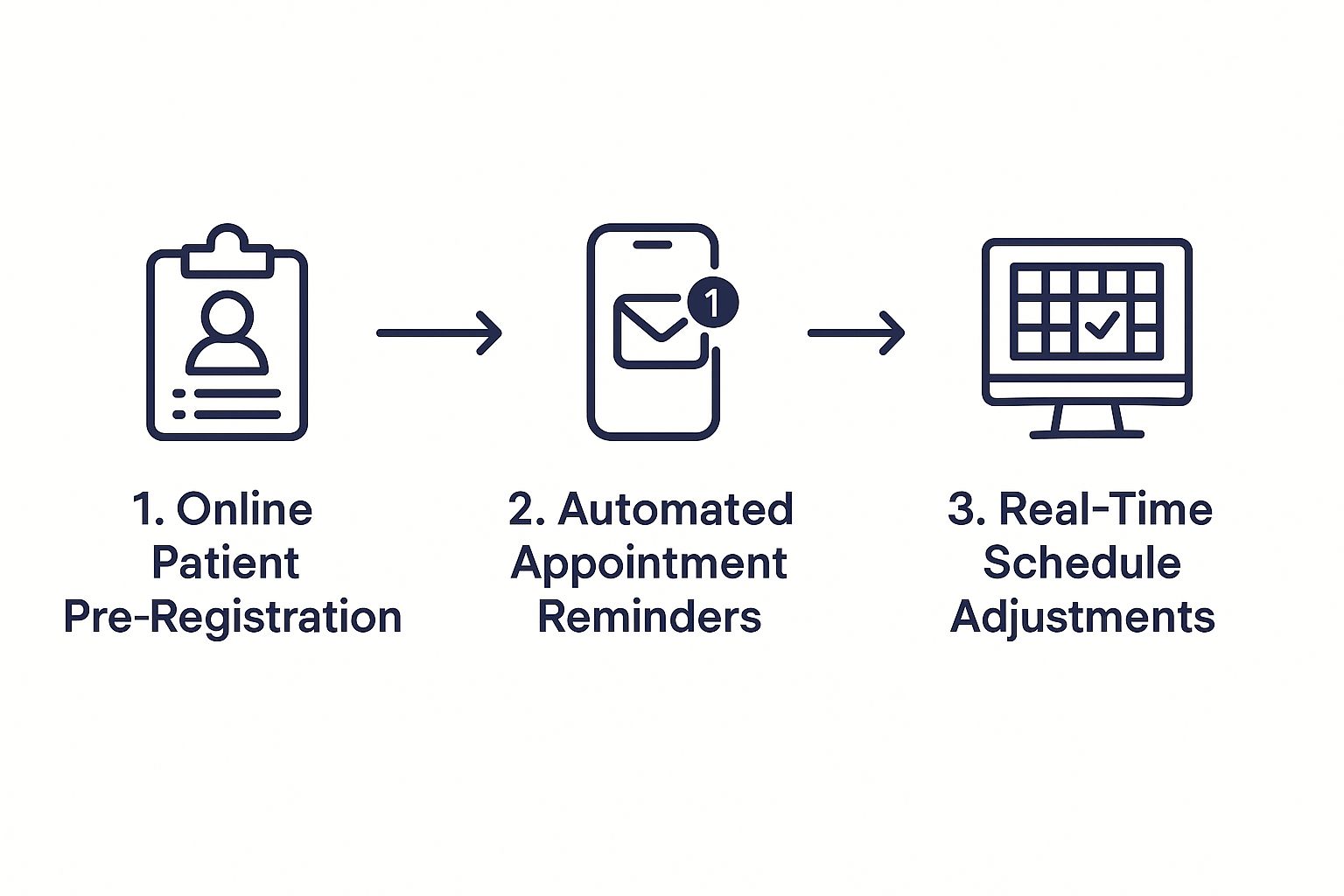
The infographic above shows a smoother patient flow using online pre-registration, automated appointment reminders, and real-time schedule adjustments. Implementing these three key steps can significantly reduce wait times and boost overall efficiency. These seemingly small tweaks create a ripple effect, improving the entire patient experience from booking to departure.
This is where we shift from identifying wait time problems to actually fixing them. I’ve seen practices dramatically reduce wait times without adding staff, and I'm excited to share these strategies. Forget theory – this is about practical, actionable advice.
Redesigning Your Workflow For Efficiency
One major cause of long wait times? A clunky, outdated workflow. Think about it: redundant check-in procedures, poorly designed patient forms, and inefficient staff scheduling all contribute to unnecessary delays. I once worked with a clinic where patients filled out the same information multiple times – online, then again on paper. Digitizing their intake process saved precious minutes per patient.
Another frequent problem is the "one-size-fits-all" appointment schedule. A quick follow-up shouldn't get the same time slot as a complex new patient consultation. Spacing appointments strategically, based on visit type, makes a huge difference. This allows for more accurate scheduling, preventing one delayed appointment from derailing the entire day.
Let's take a look at some common workflow improvements and their impact:
To help visualize the impact, here's a table summarizing the effects of these common workflow optimizations:
| Workflow Change | Implementation Difficulty | Average Wait Time Reduction | Patient Satisfaction Improvement |
|---|---|---|---|
| Online Pre-Registration | Easy | 10-15 minutes | 15-20% |
| Automated Appointment Reminders | Easy | 5-10 minutes | 10-15% |
| Staggered Appointment Scheduling | Medium | 15-20 minutes | 20-25% |
| Streamlined Check-In Process | Medium | 5-10 minutes | 5-10% |
| Integrated Patient Portal | Hard | 10-15 minutes | 15-20% |
As you can see, even simple changes like online pre-registration can have a significant impact. The more complex changes, while harder to implement, offer even greater potential for improvement.
Empowering Your Staff
Even the best plans need staff buy-in. Involving your team in the redesign process is essential. When staff understand the why, they’re more likely to embrace new procedures. Explain how shorter wait times benefit everyone – patients and staff – by reducing stress and workload. This creates a shared goal and fosters collaboration.
Clear communication is also key. Provide thorough training on new workflows and address any concerns upfront. Regular team meetings to discuss progress and identify improvement areas keep everyone engaged and accountable. By empowering your staff, you're not just implementing a new system; you’re building a culture of efficiency and patient-centered care. These changes, paired with smart technology like Simbie, can truly transform your practice. Remember, reducing patient wait times is an ongoing journey, not a one-time fix.
Smart Technology That Actually Makes A Difference

Let's face it, technology can be a double-edged sword. I've seen practices pour money into fancy systems that end up as expensive paperweights. But I've also seen surprisingly simple solutions make a huge difference in reducing patient wait times.
What if you could predict rush hour before it happened? What if your scheduling system could adapt to different appointment types? That's the promise of smart technology implemented thoughtfully.
Predictive Analytics: Knowing What's Coming
Savvy clinics are using predictive analytics to forecast busy times. It's not magic, it's just smart use of data. Think of a pediatrician’s office in October. They know flu season is coming, and appointments will skyrocket. Using this historical data, they can adjust staffing and maybe even extend clinic hours to keep things running smoothly.
This data-driven approach shifts us from reacting to problems to anticipating them. It's about getting ahead of the curve and allocating resources effectively before bottlenecks appear.
Automating the Schedule: Smoothing Out the Flow
Automated scheduling tools can be a real game-changer. They don't just book appointments, they optimize the entire flow. A quick follow-up shouldn't occupy the same slot as a lengthy first consultation. These systems adjust appointment lengths automatically, making sure each visit has the time it needs, reducing delays from overbooking and ensuring a more predictable schedule. That translates to a smoother flow for both patients and staff.
Some systems even integrate with your Electronic Medical Record (EMR) software. They automatically pull patient information and can even flag potential scheduling conflicts. This frees up staff to focus on what truly matters – patient care.
AI-Powered Communication: Keeping Everyone Informed
Keeping patients informed is essential, especially when delays are inevitable. AI-powered communication tools can proactively update patients. A quick text message letting someone know their appointment is running 15 minutes late due to an emergency can make a world of difference. It manages expectations and minimizes frustration.
Speaking of AI, you might want to check out Simbie AI’s scheduling optimization and AI voice agents. Combining streamlined workflows with these types of smart technologies can completely change how you manage wait times and improve the overall patient experience. It's a win-win for patients, staff, and your practice.
Turning Waiting Into A Positive Patient Experience
Let's be honest, waiting is nobody's favorite activity. But here's the thing: sometimes, how patients feel about the wait matters more than how long they actually wait. I've seen practices with objectively longer wait times receive glowing patient satisfaction scores, simply because they mastered the art of making patients feel valued and informed. We're going to unpack how to change the waiting game, even if the clock keeps ticking.
The magic formula? Practices that nail this use proactive updates, transparent communication, and strategic comfort measures to keep patients happy, even when delays are unavoidable. For example, one clinic I worked with implemented text message updates when a provider was running behind. Something as simple as, "Dr. Smith is running 15 minutes behind due to an emergency, we apologize for the delay," made all the difference. Patients felt respected and appreciated the heads-up, allowing them to adjust their own schedules instead of feeling stuck.
Setting Expectations and Handling Conflicts
One of the biggest secrets to managing wait times is setting realistic expectations right from the start. Let patients know upfront that unexpected delays can occur. Honesty about potential wait times during scheduling sets the stage for understanding and minimizes frustration later on. Our guide on patient appointment reminders offers some great tips on proactive communication.
Of course, even with the best planning, conflicts still happen. When they do, handle them with grace. A sincere apology and a brief explanation can work wonders. A small gesture, like a complimentary beverage, can also diffuse tension. I even saw a practice offer a small discount on future services after a major scheduling hiccup. It wasn't about the money; it was about acknowledging the inconvenience and showing patients their time was valued.
Creating a Welcoming Waiting Area
The waiting room is the first impression, so make it count. A comfortable and well-designed space can significantly reduce stress. Think calming colors, comfy seating, and engaging reading material. Simple additions like free Wi-Fi and charging stations can also make a big impact.
I’ve witnessed firsthand the positive effects of even small, budget-friendly improvements. Adding plants, playing calming music, or even installing an aquarium can transform a sterile waiting room into a more welcoming environment. The aim is to shift the perception from a place of anxiety to a comfortable pause in their healthcare journey.
Turning a potentially negative wait into a positive experience strengthens patient relationships and fosters loyalty. It's all about showing you care, even before the appointment begins.
Building Wait Time Solutions That Grow With You
I've seen firsthand how a system that works perfectly for a small practice can completely fall apart when that practice expands to multiple locations or sees a significant increase in patients. Helping organizations navigate that growth without losing their hard-won efficiency is a big part of what I do. So, let's dive into building adaptable wait time solutions that can actually evolve alongside your practice.
Think about a simple sign-in sheet. For a solo practitioner, it's probably fine. But picture that same sheet in a busy multi-specialty clinic. Total mayhem, right? This is where scalable processes become absolutely essential. As your patient volume grows, your staff changes, and your services expand, your systems need to keep pace. It’s like building a house – you can't add a second story without a solid foundation.
Healthcare wait times are a global issue, which underscores the need for adaptable solutions. It's pretty shocking: in many countries, patients are waiting months for specialist appointments. A report showed over half the countries surveyed had wait times nearing two months or more, with some like Canada and Spain hitting four months or even longer. It's worth checking out the data on global wait times.
Scaling Up Without Sacrificing Efficiency
I've seen some really clever, yet simple, changes make a world of difference. One clinic I worked with ditched their paper-based system for a centralized digital check-in kiosk. Just that one change streamlined the whole process, cut down on paperwork, and allowed them to handle a much larger patient volume without needing to hire more administrative staff.
Another practice I know adopted a modular approach to scheduling. They set up standardized time blocks for different appointment types but built in flexibility to adjust based on provider availability and individual patient needs. This made it super easy to scale their schedule up or down without messing with the patient flow.
Balancing Standardization and Flexibility
Standardization is crucial for efficiency, but too much rigidity can actually hinder growth. The trick is finding the sweet spot. A large health system I consulted with standardized their patient intake forms across all their locations, which really streamlined data collection. But, they smartly allowed individual departments to customize certain fields on those forms to fit their specific needs. This gave them the best of both worlds: consistency and flexibility.
Planning for the Future
When you’re looking at your systems, think long term. Ask yourself: "Will this still work if we double our patient volume? What happens if we open a new location or add a new service?" I've seen practices invest in systems that worked beautifully at first, but quickly became major bottlenecks as they grew. It's all about choosing solutions that aren't just efficient today, but are adaptable for the future. Building in that flexibility from the get-go saves you a lot of headaches (and money) in the long run. Because, let’s be honest, sustainable solutions are always the winners.
Your Implementation Roadmap For Real Results
Okay, so let's get down to brass tacks. Forget generic templates – this roadmap is custom-built for your practice to cut down those patient wait times. We're going to zero in on the strategies that deliver the quickest results, complete with clear timelines and ways to actually see how you’re doing. I'll even throw in some checklists for staff training and communication templates, because just knowing what to do isn't enough. It’s how you implement these changes in the whirlwind of healthcare that really makes the difference.
Prioritizing For Maximum Impact
Don’t try to boil the ocean. Go for the low-hanging fruit – those easy wins that make a noticeable impact fast. For example, if patient intake is a bottleneck, start with online pre-registration. It lets patients give you all the important info before they even walk in the door, saving precious minutes at check-in. Celebrate those small victories, then move on to the next target. This keeps your team energized and builds momentum for the bigger changes down the line.
Also, pay close attention to the biggest pain points. If patients are consistently griping about long waits for certain appointments, dissect that workflow. Maybe the allotted appointment times are unrealistic, or the scheduling system isn’t designed for that particular service.
Measuring Your Progress
Tracking the right metrics is like having a compass – it shows you what’s working and what needs adjusting. Don't just look at average wait time. Perceived wait time (how long patients feel like they’re waiting) is crucial. Patient surveys can help you capture this. Keep tabs on no-show rates too, because high numbers can be a red flag for patient frustration with long waits. Here's a simple framework:
- Baseline Data: Before you change anything, measure your current performance. This is your starting point for comparison.
- Regular Check-ins: Don’t wait months to evaluate. Track progress weekly or bi-weekly so you can quickly adjust your approach.
- Patient Feedback: Regularly ask for patient feedback through surveys or feedback forms. This gives you invaluable insight into their real experiences.
Maintaining Momentum and Long-Term Success
Initial excitement can fizzle out quickly. To keep your team engaged, celebrate successes and acknowledge individual contributions. Regularly review your progress as a team and be flexible with your strategies. This creates a culture of continuous improvement and makes these changes stick for good.
Remember, reducing patient wait time is a marathon, not a sprint. Simbie AI can be a valuable partner on this journey. Check out Simbie AI's website to see how their AI-powered solutions can help you optimize your workflows, improve patient communication, and create a more efficient, patient-centered practice.

