Why Nursing Report Templates Transform Your Practice
Let's be honest, nursing report templates aren't just about ticking boxes. They're about making sure everyone's on the same page, reducing those heart-stopping near misses, and ultimately, giving our patients the best possible care. Think about those frantic shift changes – the rushed conversations, the scribbled notes, that nagging feeling you’ve missed something vital. A well-designed template changes all that. It transforms those hectic handovers into smooth, efficient transitions of crucial information.
I’ve spoken to so many charge nurses and seasoned RNs who initially pushed back against standardized reporting. It felt too rigid, impersonal, or just another admin headache. But once they saw the benefits firsthand? They became the biggest champions. Fewer overlooked details, clearer communication with colleagues, and—get this—more time for direct patient care. That's the real magic of a good nursing report template.
For example, imagine a patient’s allergy accidentally gets left out during a verbal report. Yikes. A standardized template with a dedicated field for allergies significantly reduces that risk. We’re not just talking about avoiding errors; we’re talking about building a safety net for both patients and nurses. The right template can be a game-changer in limiting liability, too. Want to dive deeper into process improvement? Check out Simbie's guide to process improvement.
This move towards standardized reporting is gaining serious traction across healthcare. The American Hospital Association found that about 70% of hospitals in the US are already using some form of it to improve care coordination and minimize errors. That speaks volumes. Learn more about nursing report sheets. These templates aren’t about generating more paperwork; they're about creating a system where essential patient data is consistently recorded and readily accessible, which leads to a safer, more efficient environment for everyone. What this all means is that using a nursing report template isn't just a best practice anymore – it’s quickly becoming the standard of care.
Designing Your Perfect Nursing Report Template
Let's be honest, those generic nursing report templates? They just don't cut it. They're like trying to squeeze into a pair of shoes two sizes too small. Instead, let's talk about crafting a nursing report template that actually fits your unit's needs.
Seasoned charge nurses, the ones who've seen it all and done it all, know the secret: a good report is like a well-oiled machine. They understand how to make crucial info pop out during a code while keeping the routine stuff organized and easy to find. This means less time hunting and more time focusing on what matters most: your patients.
One of the biggest takeaways from these experienced nurses? Prioritization is everything. What absolutely has to be communicated during shift change? Allergies, recent labs, any changes in patient status – those are your must-haves. Everything else should support these core pieces without creating extra noise. Sure, intake and output is important, but it shouldn't bury a critical change in a patient's breathing pattern.
Smart Shortcuts and Specialty Considerations
This is where those clever little shortcuts come into play. Veteran nurses develop tricks to capture information quickly and efficiently. Think color-coding systems for urgency levels or abbreviations everyone on the team understands. These little tweaks can make a world of difference when you're juggling multiple patients and facing tight deadlines.
And don't forget about specialties! A cardiac nurse needs to highlight different information than a psych nurse. Your nursing report template should reflect the unique focus of your unit. A cardiac nurse might need to emphasize rhythm changes, while a psych nurse might zero in on behavioral observations.
Before we dive into real-world examples (which are coming soon!), let's look at a handy table to break down the essential components of an effective nursing report template. It compares must-have elements with optional ones across different nursing units.
Let's take a look at the table below, "Essential Components of Effective Nursing Report Templates," which compares must-have and optional elements across different units like Med-Surg, ICU, and the ER. This will help you visualize the differences and tailor your template accordingly.
| Component | Priority Level | Med-Surg Use | ICU Use | ER Use |
|---|---|---|---|---|
| Patient Demographics | Must-Have | X | X | X |
| Allergies | Must-Have | X | X | X |
| Current Medications | Must-Have | X | X | X |
| Code Status | Must-Have | X | X | X |
| Primary Diagnosis | Must-Have | X | X | X |
| Recent Vital Signs | Must-Have | X | X | X |
| Intake and Output | Must-Have | X | X | X |
| Plan of Care | Must-Have | X | X | X |
| Significant Events | Must-Have | X | X | X |
| Pending Labs/Tests | Must-Have | X | X | X |
| IV Access/Fluids | Must-Have | X | X | X |
| Pain Level/Management | Must-Have | X | X | X |
| Neurological Assessment | High | X | X | X |
| Respiratory Status | High | X | X | X |
| Cardiovascular Status | High | X | X | X |
| GI/GU Status | High | X | X | X |
| Skin Integrity | High | X | X | X |
| Wound Care (if applicable) | Conditional | X | X | X |
| Drains/Tubes (if applicable) | Conditional | X | X | X |
| Isolation Precautions (if applicable) | Conditional | X | X | X |
| Fall Risk Assessment | Must-have | X | X | X |
| Mobility Status | Must-have | X | X | X |
| Family/Caregiver Involvement | Optional | X | X | X |
| Social Work Consultations | Optional | X | X | |
| Physical/Occupational Therapy | Optional | X | X |
As you can see, while some components are universal, others are more specific to certain units. This highlights the importance of adapting your template to fit your specific needs.
Later, we’ll dive into specific examples from different specialties. This will give you a concrete idea of how these principles work in action and help you create a template that truly reflects your unit's unique workflow and patient population.
Adapting Templates For Different Nursing Specialties

A nursing report template designed for the ICU isn't going to work well in pediatrics. Think about it – the needs are just completely different. The same goes for using an ER template in long-term care. Each specialty has its own unique flow, terminology, and priorities.
What works in one area just won't cut it in another.
Tailoring Information Hierarchy and Assessment Categories
This is where customization is essential. You don't need to start from scratch, but you do need to adjust the template to fit your specific needs. Think of it like adjusting a bike seat – you’re not building a new bike, you’re just making it comfortable for you. The basic information – patient demographics, allergies, medications – stays the same, but the focus changes.
For example, a cardiac nurse is zeroed in on heart rhythms and hemodynamics. Their nursing report template should reflect that, putting those vital stats right up front. A psychiatric nurse, on the other hand, needs to quickly see behavioral observations, mental status exams, and medication responses. Their template should highlight those specifics.
In the ICU, a detailed neurological assessment is crucial. In pediatrics, it's all about developmental milestones and growth charts. These differences need to be reflected in how the template is organized. What's at the top? What jumps out at you first? Those are your specialty-specific priorities.
In long-term care, the focus shifts again. Here, it might be functional status, skin integrity, and cognitive changes. The nursing report template should make it easy to track these things over time, painting a clear picture of the resident's progress.
Handling Specialty Populations and Complex Cases
Another critical piece of the puzzle is your patient population. A neonatal ICU template looks nothing like one used in a geriatric unit. The terminology, the assessments, even the normal vital sign ranges, are all tailored to the specific age group.
Even within the same specialty, you'll have complex cases that need extra attention. A patient with multiple health issues needs a more thorough report, while a post-op patient might need specific assessments related to their surgery. Your nursing report template needs to be flexible enough to handle these variations. This flexibility allows for better documentation and more focused care.
By adapting your nursing report templates to your specialty, you make sure they're actually helpful, not a hindrance. It's about making a tool that works for you, empowering you to give the best possible care to your patients. A well-adapted template streamlines communication and promotes safer, more efficient care.
Digital Nursing Report Template Solutions That Work
Let's be honest, paper charting is outdated. But not every digital solution is an upgrade. I've seen firsthand how some electronic systems can actually make documentation more complicated. So, how do you find a digital platform that actually makes your life easier? The key is to listen to nurses who’ve been there, wrestled with those clunky systems, and come out on the other side. They know what truly matters when you're juggling a million things and the clock is ticking.
One of the biggest factors is integration with your existing Electronic Medical Record (EMR). A system that doesn't play nicely with your EMR, or requires duplicate entry, is a recipe for headaches and errors. Nurses I've talked to consistently emphasize the importance of a seamless flow of information. Ideally, your digital nursing report template should integrate directly into the patient’s chart, minimizing extra clicks and tedious data entry. You might also be interested in checking out Simbie's guide on scheduling optimization with AI voice agents.
Key Features That Make a Difference
Think about features like customizable templates, automated calculations, and built-in alerts. These can save you serious time and reduce the risk of mistakes. Imagine a system that automatically flags critical lab values or gently reminds you about pending orders. That kind of support is a game-changer when you're in the thick of a busy shift. Another essential feature? Mobile accessibility. Being able to access and update patient information from anywhere on the unit – or even from home for telehealth visits – can significantly improve your workflow.
On a broader scale, the move towards digital healthcare is happening everywhere. In fact, as of 2025, many facilities are ditching paper reports in favor of digital platforms, recognizing the flexibility and accessibility they offer. For more information, you can discover more insights on patient reporting. This shift highlights the importance of picking a digital solution that not only meets your current needs, but can also adapt to future tech advancements.
Advocating for Effective Systems
The best units don't just implement digital templates; they actively shape them to fit their unique needs. They also become champions for investing in systems that genuinely support nursing practice, rather than just ticking compliance boxes. They've figured out how to navigate the tech hurdles and persuade administrators to prioritize systems that truly benefit both nurses and patients. They've shown that investing in the right technology isn't just an expense; it's an investment in better patient care, happier staff, and a safer, more efficient work environment. This means making a compelling case for why a particular system is worth the investment, highlighting the tangible benefits – fewer errors, better communication, and more time for direct patient care.
Getting Your Team To Actually Use Your Template
You’ve poured your heart and soul into creating the perfect nursing report template. Now for the real challenge: getting your team to actually use it. This isn't about forcing a new form on them; it's about shifting habits, listening to concerns, and getting everyone on board, no matter what shift they work. Trust me, I've seen amazing templates fall flat without the right implementation strategy.
This section is packed with tried-and-true advice from charge nurses and nurse managers who've successfully navigated this tricky process. They've learned how to handle the inevitable pushback, especially from seasoned nurses with their own established routines. They also know the secrets to training that actually sticks, not just for a week, but for the long haul.
One of the best ways to demonstrate the value of your new template is to visualize its impact. The infographic below shows how a standardized format can lead to 30% faster completion times, consistent details result in 20% fewer documentation errors, and clear communication boosts patient satisfaction by 15%.
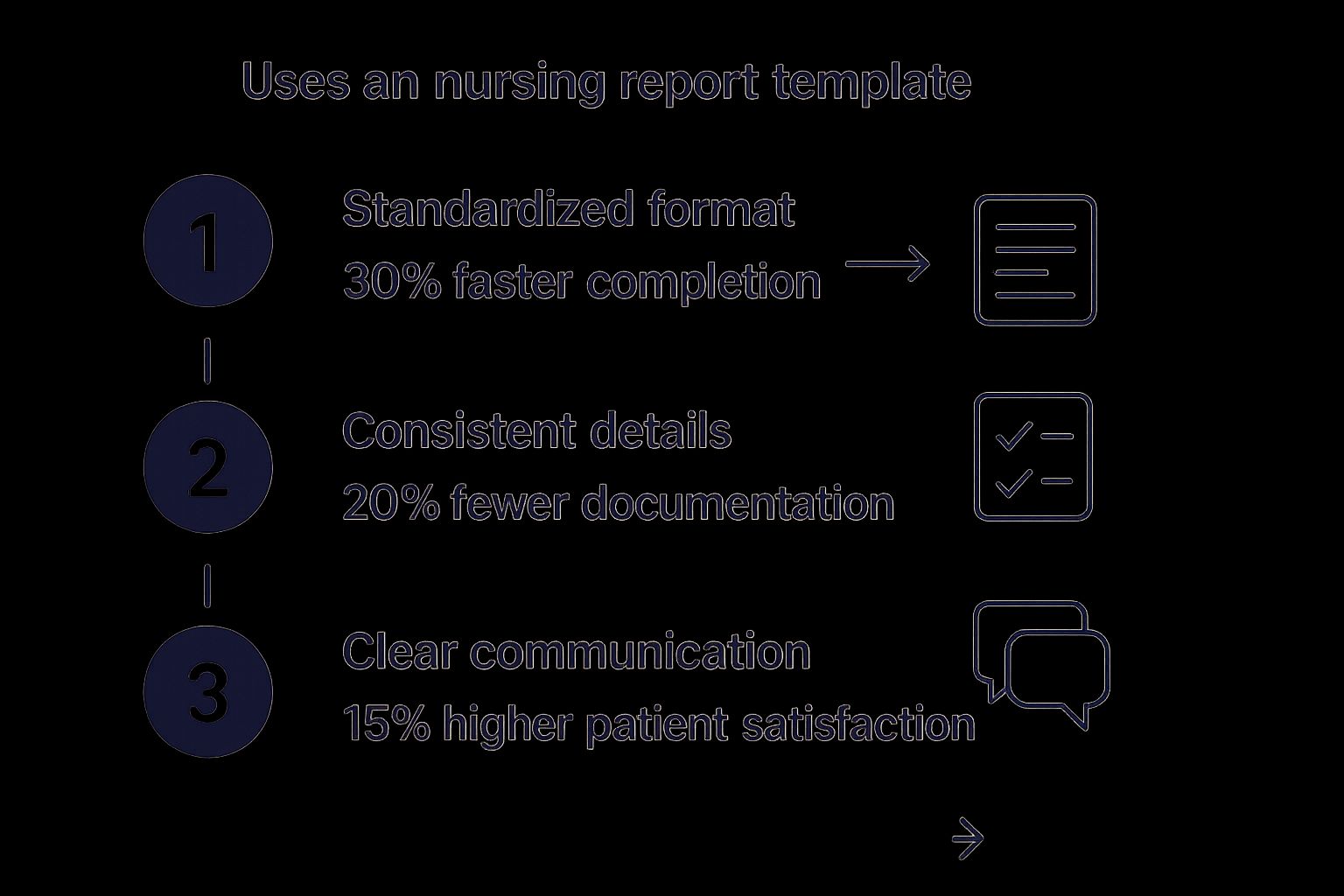
These improvements highlight the positive ripple effect of a well-implemented nursing report template. It's better for nurses, better for patients, and ultimately improves the overall quality of care. For example, a study in the Journal of Nursing Administration showed that standardized reporting significantly reduced medication errors. These real-world results can be incredibly convincing when you're trying to get a skeptical team on board.
Handling Resistance and Gathering Feedback
Let’s face it, change is tough. Experienced nurses have often honed their own systems over many years. Asking them to switch to a new nursing report template can feel like asking them to relearn a fundamental skill. The key is to respect their experience and make them part of the process from the beginning. Ask for their input, address their concerns head-on, and demonstrate how the new template can actually make their work lives easier.
Feedback is essential. But it’s not just about asking for it; it’s about creating a space where people feel comfortable sharing honest opinions. And then, just as important, acting on that feedback. This isn't a complaint box; it's a way to refine the template, making it more user-friendly and more effective for the unique needs of your unit. Actively seek out feedback, particularly from those who seem most resistant.
For some extra insights on effective communication, take a look at this helpful guide on how to reduce patient no-shows. Just like with your team, open communication and addressing concerns early on is key.
Realistic Timelines and Communication Strategies
Implementation doesn't happen overnight. Don't expect everyone to jump on board immediately. A phased rollout with clear milestones and regular check-ins can smooth the transition. Start with a small pilot group, gather their feedback, tweak the template as needed, and then gradually expand to the rest of the team. This allows everyone to acclimate to the new system at a comfortable pace. Clear, consistent communication is crucial throughout this process. Regular updates, training sessions, and readily available support can help alleviate anxiety and build confidence.
Another important tactic is showcasing the value. Demonstrate to your team how the nursing report template improves patient safety, reduces errors, and creates more time for direct patient care. These tangible benefits speak volumes more than abstract concepts like efficiency or standardization. When nurses see a direct improvement in their workflow and patient outcomes, they're far more likely to embrace the template as a valuable tool. Tracking specific metrics, like medication errors or patient satisfaction scores, before and after implementation can be a powerful way to demonstrate the positive impact.
Here's a sample timeline to help you structure your implementation:
Template Implementation Timeline and Milestones
| Phase | Duration | Key Activities | Success Indicators | Common Challenges |
|---|---|---|---|---|
| Pilot Program | 2 Weeks | Training for pilot group, initial template use, feedback collection | High template usage within pilot group, constructive feedback received | Resistance to change, initial technical difficulties |
| Revisions and Refinements | 1 Week | Incorporate feedback into the template, update training materials | Template reflects user feedback, training materials are updated | Balancing different feedback suggestions, ensuring updates are user-friendly |
| Unit-Wide Rollout | 4 Weeks | Training for remaining staff, ongoing support and monitoring | High template usage across the unit, reduction in documentation errors | Varying levels of technical proficiency among staff, maintaining momentum and enthusiasm |
| Ongoing Evaluation and Improvement | Ongoing | Regular feedback collection, periodic template reviews and updates | Continuous improvement in template usability and effectiveness, positive impact on patient outcomes | Complacency, shifting priorities |
This table provides a framework for a structured implementation process. Remember to adjust the timeline and activities based on your unit's specific needs and circumstances. The key takeaway is to approach implementation strategically, with clear communication, ongoing feedback, and a focus on demonstrating the tangible benefits for both nurses and patients.
Fixing Common Nursing Report Template Problems
So, you’re bright-eyed and bushy-tailed, ready to roll out your new nursing report template. Awesome! But here's the thing: even the slickest templates can hit a few bumps in the road. Maybe the night shift keeps skipping a section, or the template isn't quite capturing the nuances of your more complex patients. It happens. It's nursing.
This section dives into those real-world snags that pop up after implementation, sharing insights from nurses who’ve been there, done that, and found solutions that actually stick.
Information Overload and Missing Critical Data
One common issue? Information overload. A template crammed with every possible detail can quickly become overwhelming. This can lead to nurses picking and choosing what they document, or just skimming the surface. The solution? Streamline. Be ruthless. Figure out what absolutely needs to be communicated and relocate less critical info to a secondary spot. Think of it like spring cleaning your closet – the everyday essentials are front and center, while the rarely used items are tucked away.
But sometimes, vital information gets lost in the shuffle. I remember one unit I worked with where the template didn't have a dedicated section for recent lab results. This oversight resulted in several near misses before they realized the problem. The fix was simple: they added a prominent “Labs” section and highlighted critical values in bold. Small tweak, huge impact on patient safety.
Inconsistent Completion and Technology Glitches
Another headache? Inconsistent completion rates. You’ll have some nurses diligently filling out every single field, while others might take shortcuts. This creates gaps in information and sets the stage for communication breakdowns. One strategy that works is incorporating mandatory fields within your electronic health record (EHR) system. This way, key information must be entered before the report can be submitted. Regular audits are also helpful for spotting patterns of incomplete documentation and addressing any training needs.
And let's not forget the joys of technology glitches. EHR systems can be a lifesaver, but they also come with their own set of quirks. A system crash during shift change? That can throw the whole unit into chaos. Smart units have backup plans – readily available paper templates or dedicated workstations with reliable internet access. They also develop a good working relationship with their IT department to tackle recurring issues and push for system upgrades.
Addressing Compliance and Adapting to Change
Compliance isn’t optional. Regular reviews of the nursing report template are a must to ensure it aligns with current regulations and hospital policies. These reviews are also a great opportunity to get feedback from the nursing staff and pinpoint areas for improvement.
Finally, patient acuity and staffing levels are always in flux. Your template needs to be flexible enough to roll with the punches. Units that really nail this regularly evaluate their template's effectiveness and tweak it based on user feedback and evolving clinical needs. This constant refinement keeps the nursing report template a valuable, living document instead of a dusty relic everyone avoids.
Keeping Your Template Relevant and Effective

A really good nursing report template isn’t something you just create and forget. It’s constantly evolving, just like the needs of your unit. Think of it as your favorite pair of comfy shoes—reliable, and broken in over time for a perfect fit. This section is all about keeping that template fresh, useful, and learning from other units who've successfully handled changes in regulations, staff, and patient needs.
Experienced nurse managers understand that a template collecting dust does no one any good. They constantly assess its effectiveness, listen to their team’s feedback, and look for ways to improve based on quality initiatives. The goal is more than just checking boxes for administrators; it’s about providing better patient care.
Measuring Template Success and Identifying Areas for Improvement
So, how do you know if your template is working? It's not about completion rates; it’s about the impact on patients and workflow. Are medication errors decreasing? Is communication smoother between shifts? Are nurses spending less time searching for information? These are the questions to ask.
One practical tip is to track important metrics before and after using your template. For instance, monitor medication administration times, how often nurses need to clarify information, or the time spent on handoffs. This data really shows how the template is (or isn't) helping. Plus, regular chats with your nursing staff can uncover hidden problems and lead to some great improvements.
Implementing Changes and Maintaining Flexibility
Updating your template doesn’t have to be a huge disruption. Small, gradual changes are better than a complete overhaul. Perhaps it’s adding a field for a specific assessment, improving the layout, or using color-coding to show urgency.
The trick is to make your system flexible while keeping the consistency that makes standardized reporting so valuable. This could involve different template versions for various patient groups or letting nurses personalize certain sections. The goal is to create a system that helps nurses, not hinders them.
This approach also helps nurses feel more involved and see the template as a helpful tool, not just another administrative burden. When nurses contribute to its development, you build a system tailored to your unit's needs, one that continues improving over time.
Ready to take your practice to the next level with the power of voice-based AI? Explore Simbie AI today!

