Think of a medication charting template as a pilot's pre-flight checklist, but for patient care. It’s a standardized document that healthcare professionals use to track every single detail about a patient's medications. It's designed to make sure nothing gets missed and that crucial information—the right drug, dose, time, and patient—is recorded correctly, every single time. This guide explores how these templates enhance patient safety, the key components they must include, and how technology is shaping their future.
Decoding the Role of Medication Charting Templates
At its heart, a medication charting template is so much more than a log or a simple form. It’s a critical communication tool that serves as the backbone of safe patient care. By creating a consistent framework for documentation, these templates get every member of the healthcare team on the same page, ensuring that crucial information is conveyed accurately and efficiently. This level of standardization is vital for maintaining continuity of care across different shifts, departments, and even healthcare facilities.
Picture a chaotic hospital ward during a shift change. One nurse might scribble notes in shorthand, another might use a completely different format, and a third might forget a key detail altogether. This kind of inconsistency is a recipe for disaster, opening the door to misinterpretations and errors. A standardized template cuts through the chaos, establishing a single source of truth for a patient's entire medication plan. This uniformity eliminates ambiguity and ensures that every provider has access to the same, reliable information, which is a cornerstone of collaborative care.
Why Structure Matters in Medication Documentation
The real magic of a medication charting template is its structure. It transforms documentation from a messy, memory-based task into a systematic, checklist-driven process. This structured approach is absolutely vital for a few key reasons:
- Error Reduction: Having standardized fields means critical details like allergies or specific administration times are far less likely to be overlooked. This systematic approach forces a moment of verification for each critical data point.
- Improved Communication: When everyone uses the same format, handoffs between shifts or departments become incredibly smooth and clear. The information is presented in a predictable layout, allowing for faster comprehension and reducing the risk of miscommunication.
- Enhanced Consistency: Every patient's medication record follows the same logical flow, which makes it easy for any provider to quickly grasp their history and current treatment. This is particularly important for patients with complex medication regimens.
- Legal Protection: A well-kept chart is a clear legal record of the care provided, which protects both the patient and the healthcare provider. It serves as indisputable evidence that protocols were followed and care was administered as prescribed.
A well-designed medication chart isn't about creating more paperwork. It's about creating clarity. It turns complex medication schedules into an easy-to-read map that guides clinicians toward safe and accurate administration.
More Than a Record—It Is a Safety System
Ultimately, these templates are a fundamental safety system. In a field where a misplaced decimal point can have life-altering consequences, you simply can't afford to be disorganized. A good template helps enforce the "Five Rights" of medication administration: the right patient, the right drug, the right dose, the right route, and the right time. It acts as a procedural safeguard, prompting clinicians to verify each of these critical elements before proceeding.
By standardizing how information is captured and displayed, medication charting templates give every clinician the exact same, unambiguous view of a patient’s treatment. This shared understanding is the cornerstone of preventing medication errors and delivering the highest quality of care possible. It creates a reliable system that supports clinical decision-making and fosters a culture of safety within the healthcare environment.
The Anatomy of an Effective Medication Chart
So, what’s the real difference between a basic medication log and a chart that truly works? It’s not just about having boxes to check. It’s about having the right boxes, each designed to protect the patient. A great medication chart is a meticulously designed tool where every single field has a purpose. It's a comprehensive document that leaves no room for ambiguity or error.
Think of it as the blueprint for a building. Every line and measurement is there for a reason, making sure the final structure is safe and sound. A medication chart is no different—each section is a building block for patient safety, heading off miscommunication and preventing dangerous errors before they happen. The design must be intuitive, logical, and comprehensive to be effective in a high-pressure clinical setting.
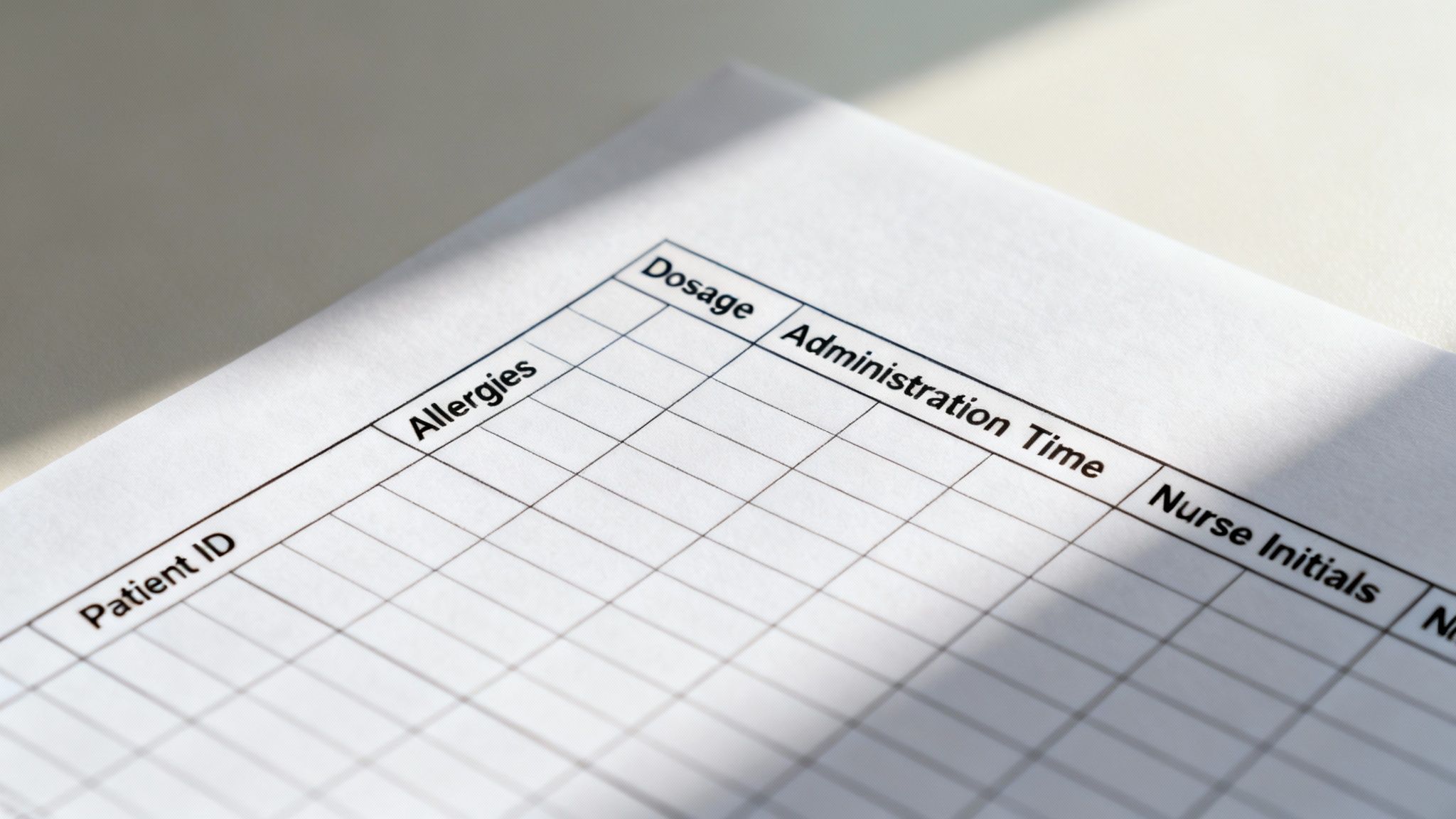
H3: Core Patient Identifiers
Before a single pill is dispensed, we have to know exactly who the patient is. This is the absolute first line of defense against mix-ups, which can be devastating in a busy hospital or clinic. There's no room for guesswork. Accurate patient identification is a fundamental safety standard recognized globally.
To get this right, every template needs these non-negotiable fields:
- Patient's Full Name: Spelled out clearly to avoid any confusion with others. This should include both first and last names, and a middle initial if available.
- Date of Birth (DOB): The classic secondary check to confirm you've got the right person. It's a universally accepted identifier.
- Unique Medical Record Number (MRN): This is the ultimate failsafe, a facility-specific ID that separates patients who might share a name and birthday.
These three pieces of information work together like a lock and key, ensuring the care documented on the chart goes to the right person. Every single time. This multi-factor identification process is critical for preventing wrong-patient errors.
H3: Critical Clinical Information
Once we’ve confirmed the patient’s identity, the chart needs to show a quick snapshot of their most important clinical details. This is the context that drives safe medication decisions and helps prevent adverse reactions. Just listing meds is only half the story; understanding the patient's clinical background is equally important.
A truly robust template will always feature space for:
- Known Allergies: This needs to be impossible to miss. Think bold red text or a color-coded box that screams "pay attention!" It should be prominently displayed at the top of the chart.
- Primary Diagnosis: Knowing why the patient is being treated helps make sense of the medications they've been prescribed and allows for better clinical judgment.
- Relevant Medical History: Conditions like kidney or liver problems can dramatically change how a person's body processes a drug, making this information absolutely critical for dosing and drug selection.
This data acts as a set of clinical guardrails, steering providers toward the safest choices. Looking at a complete patient medical chart example can be a great way to see how all these different elements come together in a real-world format.
H3: Detailed Medication And Administration Protocols
Now we get to the heart of the chart: the administration record. This section demands absolute precision. It's the legal and clinical proof of what was given, when it was given, and who gave it. Meticulous documentation here is non-negotiable.
The rule in healthcare is simple but powerful: If it wasn't documented, it wasn't done. Accurate charting is the only proof of care we have.
To make sure everything is captured, the best templates are built around a clear table structure. The goal is to provide a complete picture at a glance, leaving no room for interpretation.
Here’s a breakdown of the must-have components in any medication administration record (MAR):
Essential Components of a Medication Charting Template
| Component | Purpose | Example |
|---|---|---|
| Medication Name | To avoid confusion, includes both generic and brand names. | Acetaminophen (Tylenol) |
| Dosage | Specifies the exact strength of the medication. | 500 mg |
| Route | Shows how the medication is to be administered. | PO (by mouth), IV (intravenous) |
| Frequency | Dictates the timing of scheduled doses. | q8h (every 8 hours), BID (twice daily) |
| Time & Initials | Creates accountability and a legal record of administration. | 09:00, RN |
| Patient Response | A space to note any effects or adverse reactions. | "Pain decreased from 8/10 to 3/10" |
On top of the scheduled medications, a separate section for PRN (as-needed) medications is crucial. This part must clearly state the reason for giving the dose (e.g., "for nausea" or "for pain rated 7/10 or higher") to ensure it's used appropriately. Each of these details works together to create a complete, legally sound record that puts patient well-being first.
How Standardized Templates Improve Patient Safety

Imagine walking into a hospital where every nurse charts medications in their own unique way. One might use personal shorthand, another might list drugs by time, and a third could group them by drug class. At shift change, the next nurse has to become a detective, wasting precious time just trying to figure out what happened an hour ago.
This isn't just a headache; it's a huge safety risk. When documentation is all over the place, the chance of a misstep skyrockets. A misplaced decimal point, a confusing abbreviation, or a missed allergy note can easily lead to a serious—or even fatal—medication error. These inconsistencies create a fertile ground for human error.
This is where standardized medication charting templates come in. They create a universal language for everyone on the care team, ensuring that every provider records and reads critical information the exact same way. This consistency is the bedrock of patient safety, minimizing variability and promoting reliable practices.
Reducing Cognitive Load on Staff
Think about the immense pressure on healthcare professionals. They make critical decisions all day long. A template provides a consistent structure, which means they spend less mental energy figuring out how to document and can focus entirely on what they are documenting. By automating the format, it frees up cognitive resources for more complex clinical thinking.
It’s a lot like a pilot’s pre-flight checklist. Pilots don't have to reinvent the safety process every time they enter the cockpit; they follow a trusted, step-by-step procedure. This systematic approach is proven to minimize human error, whether you're at 30,000 feet or at a patient's bedside. Templates bring this same level of procedural discipline to healthcare.
Preventing Life-Threatening Errors
A well-built template is more than just a form; it's a safety net. It puts the most important information in predictable places, making it far easier to spot potential conflicts or catch something that was missed. It's a proactive tool for risk mitigation.
- Clear Allergy Alerts: Good templates have dedicated, often color-coded, sections for allergies that are impossible to miss. This visual cue immediately draws attention to critical safety information.
- Uniform Dosage Formats: By requiring consistent units (like mg vs. mcg), templates help prevent some of the most catastrophic dosing errors. This eliminates a common source of ambiguity.
- Structured Handoffs: During a busy shift change, a standard chart makes the transfer of information quick, accurate, and complete. This ensures nothing falls through the cracks and maintains continuity of care.
A standardized medication chart is more than a piece of paper or a screen. It’s a system-level safety tool. It turns a collection of individual notes into a single, reliable record that everyone can trust.
A Foundation for Better Teamwork
Clear communication is everything in healthcare, and standardization is the key. When a pharmacist, a doctor, and a nurse are all looking at the same structured document, they are working from a single source of truth. This shared understanding is vital for complex tasks, and you can see its impact in the medication reconciliation process. It fosters interdisciplinary collaboration and ensures all team members are aligned.
This idea is especially important as more health systems go digital. The adoption of electronic medical records (EMRs) worldwide depends on well-designed templates to make documentation easier. Research shows that doctors are more likely to embrace new EMR systems if they are easy to use. An intuitive, simple charting template gets used correctly, which directly improves patient safety. The usability of the interface is directly linked to the quality and accuracy of the data entered, making template design a critical factor in the success of EMR implementation.
Ultimately, by getting rid of ambiguity and creating a reliable system, medication charting templates do more than just keep things organized—they actively save lives. They are an essential component of a high-reliability healthcare organization.
Customizing Templates for Your Clinical Setting
Think of a standard medication charting template as a good, basic blueprint. It's a solid start, but it’s almost never a perfect fit right out of the box. After all, the frantic pace of a pediatric ER is a world away from the steady routine of a long-term care facility. To make a template truly work, you have to customize it—to fine-tune that blueprint until it matches the real-world demands of your clinic and your team.
This isn't about reinventing the wheel. It's a careful balancing act. You want to keep the core, standardized safety features but also make the document reflect the day-to-day realities of your patients and workflow. Skip this step, and even the most well-designed template can feel clunky, forcing staff into workarounds that defeat the whole purpose of having a safe system in the first place. These workarounds often introduce new, unforeseen risks.
Why One Size Does Not Fit All
Every clinical environment has its own unique rhythm, priorities, and risks. A pediatric unit, for example, lives and breathes by weight-based dosing—a detail that's a complete non-issue in most adult primary care settings. If your template doesn't account for these specifics, you're leaving dangerous gaps in your documentation. Context-specific design is crucial for maximizing both usability and safety.
Just look at how different the needs can be:
- Pediatric Units: It's non-negotiable. You need fields for the patient's weight and the calculated dose to prevent devastating errors. These fields should be mandatory to ensure compliance.
- Geriatric Facilities: A simple "Can/Cannot Be Crushed" checkbox is a lifesaver when many residents struggle with swallowing pills. This small addition can prevent choking hazards and ensure proper administration.
- Oncology Clinics: These charts must track intricate details like chemotherapy cycle numbers, dates, and very specific infusion protocols. The complexity of these regimens demands highly specialized templates.
- Mental Health Wards: It’s helpful to have a dedicated spot to note how a patient is responding to psychotropic drugs, including changes in mood or behavior. This allows for better monitoring of therapeutic effects and side effects.
Each of these examples shows just how quickly a generic template falls short. Customization isn't about preference; it's about building in practical safeguards for the specific people you care for every day.
Conducting a Practical Needs Assessment
Before you touch a single field, you need to understand what your team actually needs on the ground. A good needs assessment is the foundation for any successful customization. This doesn't have to be a big, formal affair. It's really just about asking the right questions and, more importantly, listening to the answers from the people on the front lines. Their direct experience provides invaluable insight.
Start by getting your end-users in a room—the nurses, medical assistants, and doctors who will be using this chart constantly. Their hands-on experience is gold. Create a collaborative environment where they feel comfortable sharing honest feedback.
Ask them direct, practical questions to get to the heart of the matter:
- "What do you always end up scribbling in the margins because there’s no spot for it?" This instantly tells you what fields are missing and reveals common workarounds.
- "Which parts of our current chart are confusing or always seem to get filled out wrong?" This highlights areas that need to be simpler or clearer, pointing to design flaws.
- "What's the single biggest medication risk we face with our patients?" This helps you prioritize which new fields will have the most impact on safety.
When you bring your team into the process like this, you don't just get a better template. You get their buy-in, which makes them far more likely to actually use it correctly and consistently. This collaborative approach fosters a sense of ownership and encourages adoption.
Designing and Testing Your Custom Template
Once you have a clear picture of what's needed, you can start tweaking the design. The key here is to make small, deliberate changes. Don't try to overhaul everything at once. Focus on adding or adjusting the fields that solve the biggest problems you uncovered in your assessment. An iterative design process is often the most effective.
A great custom template makes the right thing to do the easy thing to do. If a piece of information is critical for safety, the field for it must be obvious, clear, and quick to fill out.
After you've updated your medication charting templates, the next step is absolutely crucial: pilot testing. Don't just roll it out to everyone and hope for the best. Pick a single unit or a small group of clinicians and have them use the new template for a week or two.
This trial period is your chance to see how it works in the real world. Is the new layout actually intuitive? Do the new fields slow things down too much? Does it print properly? Get feedback from the pilot group, make your final tweaks, and then roll it out facility-wide. This simple, iterative process is what ensures your new template isn't just compliant, but genuinely useful. It validates the design in a real clinical context before a large-scale implementation.
The Future Is Digital and AI-Powered Charting

The days of wrestling with paper charts and messy clipboards are numbered. The way we track medications is going digital, with medication charting templates built right into Electronic Health Records (EHRs). This isn't just about swapping paper for screens; it’s about making the whole process smarter and safer. The transition represents a fundamental shift from static records to dynamic, interactive systems.
Digital templates are active safety nets, not just static records. Think about it: when a clinician enters a new prescription, the system can instantly check it against the patient's allergies and current medication list. Paper could never do that. This real-time clinical decision support is a game-changer for patient safety.
This introduces some powerful new safeguards:
- Automated Drug Interaction Alerts: The system flags potentially dangerous combinations before a single pill is administered, preventing adverse drug events.
- Real-Time Data Access: A doctor in their office can see the exact medication a nurse gave at the bedside just moments ago, improving communication and coordination.
- Standardized Dosing Guidance: Templates can have built-in clinical guidelines to help prevent common dosing mistakes, promoting evidence-based practice.
This instant feedback and built-in intelligence cuts down on human error and keeps the entire care team on the same page, allowing for much more proactive patient care.
The Rise of AI in Clinical Documentation
Digital EHRs were a huge step forward, but the next big jump is happening now with Artificial Intelligence. AI is completely changing the game for medication charting, turning it from a manual data-entry chore into an automated, intelligent process. The goal is simple: let clinicians focus on their patients, not on paperwork. This shift aims to reduce administrative burden and combat clinician burnout.
As we move toward AI-powered charting, it's also worth looking at how specialized dictation software for medical professionals can ease the transition. This tech lets clinicians dictate their notes, which dramatically cuts down on the time spent typing into an EHR, making documentation faster and more natural.
AI is transforming the medication chart from a historical record into a predictive tool. It can analyze patterns in a patient's data to flag risks before they become emergencies, creating a new layer of proactive patient safety.
How AI Is Changing the Game
AI does more than just turn speech into text. It’s about making sense of all the unstructured data—like conversation notes—and turning it into useful clinical information. To really get a feel for this, you can explore the world of AI clinical documentation and see how these tools are already being used in practices today. This technology bridges the gap between natural human interaction and structured data requirements.
New AI technologies are bringing incredible capabilities to the table:
- Automated Data Entry: Some tools can now listen to a conversation between a patient and a doctor and automatically fill out the right fields in the medication chart, reducing manual input.
- Predictive Analytics: By analyzing data from thousands of patients, AI can spot individuals who are at high risk for bad reactions to a drug, paving the way for early intervention and personalized medicine.
- Intelligent Summarization: AI can generate a quick, easy-to-read summary of a patient's entire medication history in seconds, which is invaluable for clinical handoffs and reviews.
A perfect example is the rise of "ambient scribes"—AI tools that turn spoken conversations into structured clinical notes. This technology is catching on fast. One health system reported saving 15,000 hours after rolling it out, giving that time back to clinicians to spend with patients. The research on AI adoption in healthcare delivery shows a clear trend: we're heading toward a future where technology handles the documentation, so humans can focus on healing.
Getting New Templates into Practice the Right Way
A perfect medication charting template is useless if nobody uses it correctly. The rollout is everything. A thoughtful implementation plan is the difference between a great idea that collects dust and a tool that genuinely improves how your team works. Successful adoption requires more than just a good design; it demands a strategic approach to change management.
Think of it this way: you wouldn't just drop a new, life-saving piece of equipment in a corner and expect your staff to figure it out. You’d show them why it matters, give them hands-on training, and make sure they understand how it makes their jobs safer and more efficient. The same goes for a new charting system. Proper education and support are critical for success.
Start by Getting Your Team on Board
Let's be honest, the biggest hurdle for any new process is resistance to change. Your staff is busy, and a new template can easily feel like just another administrative burden. That's why the very first step is getting them to buy into the idea. Addressing the human element of change is paramount.
The best way to do this? Involve your clinical team—the people who will actually be using the template—right from the start. When they have a say in how the template is designed, they take ownership of it. It becomes their solution, not just another rule from management. This participatory approach is key to overcoming resistance.
Here’s how to build that support:
- Explain the ‘Why’: Clearly show how the new template makes patient care safer and their daily workflow less confusing. Connect the change to shared goals like patient safety.
- Show What’s in It for Them: Frame it as a tool that reduces errors during shift changes and offers better legal protection. Highlight the direct benefits to their daily work.
- Listen to Their Feedback: Ask them what their concerns are and actually address them. This shows you respect their expertise and helps you catch potential problems early on.
A Phased Rollout and Solid Training
Instead of flipping a switch and making everyone use the new template overnight, try a more gradual approach. A pilot test is your best friend here. Start with a single unit or a small, dedicated team. This lets you get real-world feedback and iron out any kinks in a controlled setting before going facility-wide. This minimizes disruption and allows for refinement.
A pilot test isn't about being hesitant; it's a smart quality-check. It makes your staff partners in perfecting the process and ensures the final version is practical and ready for everyone.
Once you've refined the template, training is an absolute must. And no, a quick email won't cut it. Host short, hands-on training sessions where staff can walk through a few patient scenarios using the new form. Give them simple cheat sheets that highlight what’s different from the old way of doing things. The more confident they feel at the beginning, the smoother the whole transition will be. Provide ongoing support and resources after the initial training.
Bringing in structured templates is really about improving clinical workflows. To get a better handle on the bigger picture of optimizing how work gets done, you can explore general guides on workflow automation principles.
This shift toward smarter, digital tools is happening everywhere in healthcare. The market for medication adherence software is booming, which tells you how much focus there is on digital solutions. It’s a global trend. In Singapore, for example, 92% of healthcare leaders said they were adopting or planning to use predictive analytics back in 2022. This push highlights just how valuable data-driven tools like well-designed charting templates really are. You can read more about these global healthcare technology trends.
Common Questions About Medication Charting Templates
When you're dealing with healthcare documentation, a lot of practical questions pop up. As teams get better at using medication charting templates, the same kinds of questions tend to surface from both clinicians on the floor and the administrators managing it all. Getting straight answers is the only way to make sure these tools are used safely and effectively. Addressing these common queries can help build confidence and ensure consistent practice.
Let’s tackle some of the most common questions head-on. These answers should clear up any confusion and help you navigate the day-to-day challenges in your own practice.
What’s the Difference Between a MAR and a Medication Charting Template?
This is probably the most common point of confusion, but it’s actually pretty simple when you break it down. Think of a Medication Administration Record (MAR) as a very specific, official document. It's the formal, legal record that tracks every single dose of medicine given to a patient. It is the final, audited document of medication events.
A "medication charting template" is the broader, umbrella term. It’s any pre-made form or layout designed for documenting medications. So, while most MARs are created from a template, not every template is an official MAR. The template is the blueprint, and the MAR is the completed, official building. The MAR is the final, legally binding proof of care.
Can I Use a Digital Charting Template on a Tablet or Phone?
Absolutely. In fact, it’s quickly becoming the norm. Modern Electronic Health Record (EHR) systems are built with mobile devices in mind, letting clinicians chart on a tablet or phone right at the point of care. This practice is often referred to as point-of-care documentation.
This isn't just a gimmick; it’s highly encouraged for a few huge reasons:
- Fewer Errors: When you document in real-time, you don't have to rely on memory. This cuts down on the risk of forgetting details or making mistakes when you finally get back to a computer. It improves data accuracy significantly.
- More Efficient: It’s a massive time-saver. No more walking back and forth to a nursing station just to finish up paperwork. This streamlines workflow and increases time available for direct patient care.
- Instant Backup: Mobile devices give you immediate access to decision-support tools, like drug interaction checkers, right at the patient's bedside when you need them most.
Of course, this all has to be done on secure networks with strict rules in place to keep patient data private and safe. HIPAA compliance and robust cybersecurity measures are non-negotiable.
What Are the Legal Risks of Incorrect Medication Charting?
The legal stakes are incredibly high, and you can't afford to take them lightly. A patient’s chart is a legal document, and there's a simple but powerful rule in healthcare: "If it wasn't documented, it wasn't done." This principle is a cornerstone of medical-legal practice.
Bad charting—whether it's inaccurate or incomplete—can directly lead to patient harm. That can open the door to malpractice lawsuits, disciplinary action from your licensing board, and in the worst cases, losing your license.
Accurate, timely, and complete charting is your number one legal defense. It’s the proof that you provided the right care and followed all the safety protocols. It demonstrates adherence to the standard of care. So, getting good at using medication charting templates isn't just about being organized; it's a core part of your legal and ethical responsibility. It protects your patient, your facility, and your own career.
Ready to cut down on administrative work and give your staff more time for actual patient care? Simbie AI puts tasks like appointment scheduling, prescription refills, and patient intake on autopilot with clinically-trained voice agents. This frees your team to focus on what really matters. See how our HIPAA-compliant platform can boost your practice's efficiency and patient satisfaction at https://www.simbie.ai.

