Why Your Medical Intake Form Is Your Healthcare Lifeline

It’s easy to view the medical intake form as just another piece of administrative work—a boring task to complete before you can see your doctor. However, this document is much more than that; it's your healthcare passport. It serves as the first and often most important communication tool between you and your care team, laying the groundwork for your entire treatment plan.
More Than Just Paperwork
Think of your intake form as the blueprint for your personal health. When filled out with care, it helps doctors avoid dangerous drug interactions, make correct decisions in emergencies, and arrive at an accurate diagnosis. A complete medication list, for example, could be the single detail that prevents a life-threatening allergic reaction. Emergency room physicians often say a detailed form provides more immediate, useful context than initial lab results.
This first point of contact has changed quite a bit over time. What were once simple handwritten pages are now frequently detailed digital systems. Today, nearly 70% of global healthcare providers use digital methods for patient intake. This is a significant jump from less than 30% a decade ago, highlighting a move toward greater accuracy and efficiency. You can find more details on these trends by exploring patient intake statistics on LLCBuddy.com. Taking this first step seriously can genuinely improve the quality of care you receive.
The Must-Have Fields That Actually Matter
A well-structured medical intake form is built on a foundation of essential questions. While some fields might seem like simple administrative details, others are critical for your safety and effective treatment. Think of it as a hierarchy: certain information is non-negotiable for providers to deliver care, while other details add valuable context to your health profile.
The most effective forms balance what is legally required with what will improve your care. This infographic breaks down the core components.
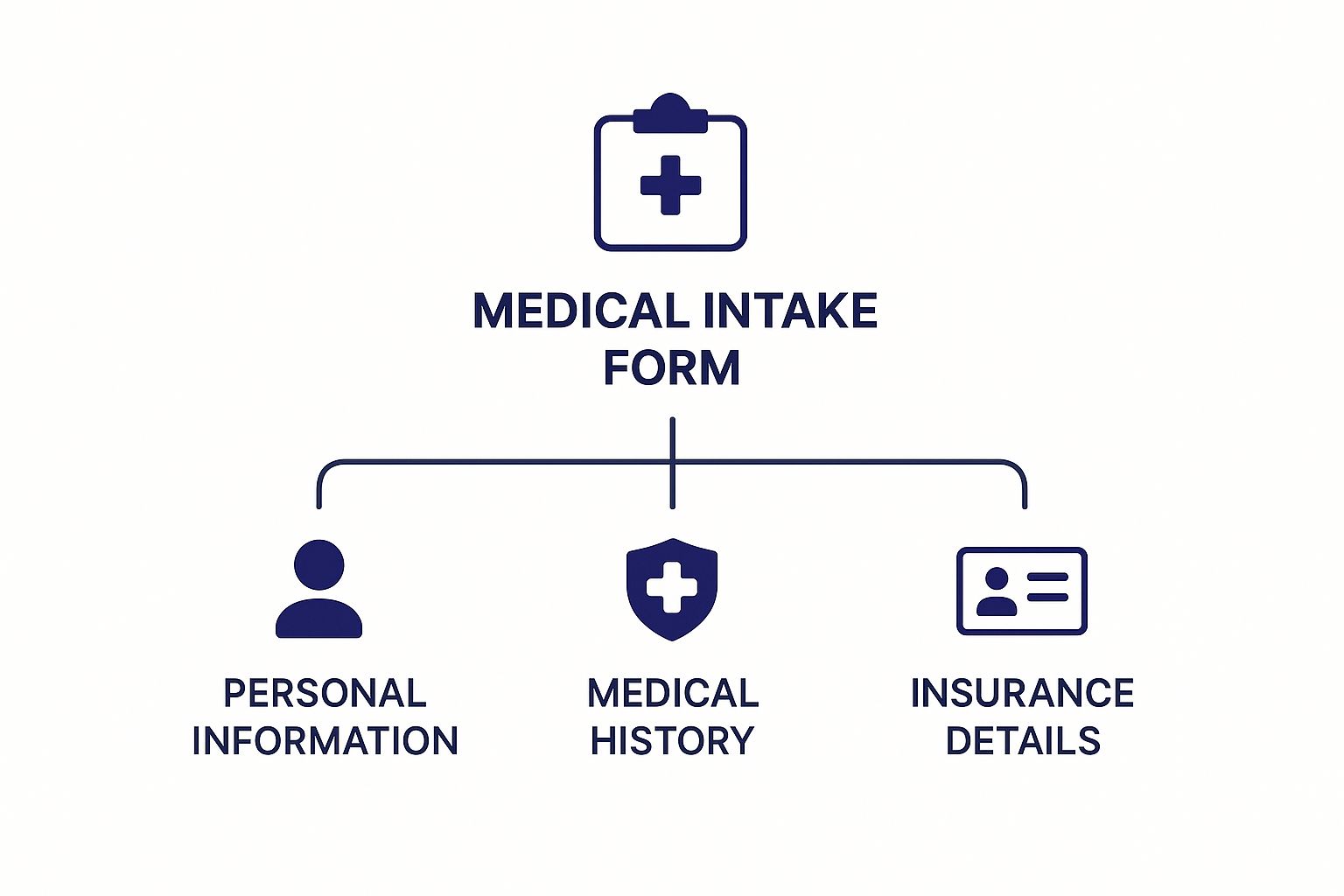
As shown, your personal, medical, and insurance information create the three pillars of any complete intake form. Leaving any of these sections incomplete can cause care delays or frustrating billing errors. For example, your current medication list is just as important as your insurance card, as it helps doctors prevent dangerous drug interactions.
Differentiating Essential from Optional Information
It's helpful to understand which fields are absolutely necessary and which ones provide a more detailed, but not mandatory, picture of your health. The following table compares these two categories to clarify what information healthcare providers need versus what they would like to have for a more complete patient profile.
| Field Category | Essential Fields | Optional Fields | Purpose |
|---|---|---|---|
| Personal & Demographic | Full Name, Date of Birth, Contact Information, Emergency Contact | Marital Status, Occupation, Preferred Language | Essential: Uniquely identifies the patient and ensures communication. Optional: Adds social context for personalized care. |
| Medical History | Known Allergies, Current Medications & Dosages, Chronic Illnesses (e.g., diabetes, hypertension), Surgical History | Family Medical History, Immunization Records, Mental Health History | Essential: Prevents adverse reactions and informs diagnosis. Optional: Helps assess genetic risks and provides a fuller health picture. |
| Lifestyle & Social | Alcohol and Tobacco Use | Diet Habits, Exercise Routines, Stress Levels, Living Situation | Essential: Identifies immediate health risk factors. Optional: Offers insight into wellness and preventative care opportunities. |
| Insurance & Billing | Insurance Provider, Policy & Group Number, Subscriber Information, Billing Address | Secondary Insurance Details, Payment Authorization | Essential: Secures payment for services rendered. Optional: Streamlines coordination of benefits if multiple plans exist. |
| Consent & Authorization | Consent for Treatment, HIPAA Acknowledgment, Financial Responsibility Agreement | Release of Medical Records to other providers, Research Participation Consent | Essential: Fulfills legal requirements for treatment and privacy. Optional: Facilitates care coordination and advances medical science. |
This breakdown shows how essential fields form the backbone of safe and compliant medical care, addressing immediate needs and legal requirements. Optional fields build upon this foundation, allowing providers to offer more holistic and preventative advice. By completing these forms accurately, you play an active role in creating a better healthcare experience for yourself. To learn more about improving the patient journey, you can check out our guide on how to improve patient satisfaction scores.
Digital Revolution: Why Electronic Forms Are Winning
Moving from paper to a digital medical intake form is more than just a modern convenience—it's a complete overhaul of how healthcare administration works. The days of trying to read messy handwriting or tracking down misplaced clipboards are fading fast. Electronic forms are taking over because they solve the biggest problems of their paper predecessors: they are more efficient, accurate, and secure.
This change greatly reduces the workload for administrative staff and shortens waiting room times. For example, a digital form can connect directly to a patient's electronic health record (EHR), doing away with repetitive questions and manual data entry. Studies show that electronic systems can decrease documentation errors by over 10%.
Plus, smart forms can automatically check for errors, making sure all essential fields are filled out correctly. This catches common mistakes that could otherwise cause delays in care. Ultimately, the entire process becomes quicker for patients and much more dependable for healthcare providers.
Privacy Protection: What Really Happens to Your Data
Your health information is deeply personal, so it's natural to wonder about privacy when you fill out a medical intake form. What actually happens to your data after you click "submit"? In the U.S., the Health Insurance Portability and Accountability Act (HIPAA) provides a strict set of rules for how healthcare organizations must handle your information. This means your data is encrypted, stored securely, and only accessible to authorized people directly involved in your care.
Your Rights and Your Data's Journey
Think of HIPAA as a digital security guard for your health story. It ensures the details on your intake form are used for their specific purpose—your treatment, payment processing, and essential healthcare operations—and not shared without your direct permission.
But the story doesn't end there. When aggregated and made anonymous, this data helps advance public health. In fact, it's estimated that by 2025, over 80% of clinical trials will use information that was first collected on forms just like these. You can discover more about how intake data advances health globally on IQVIA.com.
The Hidden Economics of Healthcare Efficiency

Think of a busy medical practice. Every minute a staff member spends on administrative work is a minute they can't spend with a patient. This is where a well-designed medical intake form becomes more than just a piece of paper—it's a tool for managing costs. When these forms are accurate and easy to complete, they directly impact the financial health of a practice and its patients.
Precise information from the start helps prevent expensive billing errors and reduces the chance of claim denials. For patients, this means fewer surprise bills. For providers, it means less time spent on correcting paperwork and more resources available for what truly matters: patient care.
The financial effects are significant when viewed on a larger scale. As healthcare expenses continue to climb, smart solutions are essential to keep costs in check. The switch to electronic intake forms has been shown to cut down paperwork processing times by as much as 30%, leading to substantial savings across the healthcare sector. You can read more about these global medical trends on WTW.com.
For any healthcare organization, fine-tuning these first interactions is a cornerstone of effective healthcare process improvement.
Best Practices for Medical Intake Forms
To make your next appointment go smoothly, it helps to understand the perspective of the healthcare professionals who will use your medical intake form. Medical assistants and nurses often suggest a simple strategy: get your information together before you even start filling out the paperwork. This means having your insurance card, a detailed list of current medications with dosages, and the contact information for your other doctors within easy reach.
How Patients Can Prepare for Success
One of the most common hurdles providers encounter is an incomplete or vague medical history. Think of your intake form as the opening chapter of your health story for that visit. Instead of just writing "heart problems," providing specific details like "atrial fibrillation diagnosed in 2022" gives your care team a much clearer picture. This level of detail is essential for accurate and safe treatment.
A few simple steps can make a huge difference:
- Be Specific: Always include precise diagnoses, dates of surgeries, and exact medication dosages. The more detail, the better.
- Don't Guess: If a question is confusing or you're unsure of the answer, it’s better to leave it blank and ask for clarification at the office. Incorrect information can be more problematic than missing information.
- Review Before Submitting: A quick final read-through can help you catch simple mistakes or typos that could otherwise lead to delays or confusion.
This process is a partnership. While patients provide the information, providers are responsible for creating forms that are easy to understand and complete. When questions are clear and concise, the answers are more likely to be accurate and useful. This collaborative approach ensures your care team gets the information they need to help you effectively. For a deeper dive into this dynamic, these healthcare communication strategies offer valuable insights.
Patient vs. Provider Best Practices
To get the best results from medical intake forms, both patients and providers have key roles to play. The table below outlines the best practices for each side, highlighting how collaboration leads to better healthcare outcomes.
| Practice Area | Patient Best Practices | Provider Best Practices | Expected Outcome |
|---|---|---|---|
| Information Accuracy | Provide specific details (e.g., "Atrial Fibrillation," "50mg Metoprolol twice daily"). | Design forms with clear, unambiguous questions and provide examples. | The clinical team receives precise data, reducing the risk of medical errors and improving diagnostic accuracy. |
| Completeness | Fill out all known sections and bring a list of questions for any unclear parts. | Create logical sections and use conditional logic in digital forms to hide irrelevant questions. | A comprehensive health history is captured without overwhelming the patient, ensuring no critical information is missed. |
| Efficiency | Gather all necessary documents (insurance card, medication list) beforehand. | Offer digital intake forms that patients can complete at home before their appointment. | The check-in process is faster, reducing wait times and administrative workload for front-desk staff. |
| Communication | Be honest about lifestyle habits and symptoms, even if they seem minor. | Ensure the form includes open-ended fields for patients to add context or ask questions. | A relationship of trust is established, and the provider gains a holistic view of the patient's health and concerns. |
| Usability & Design | Take the time to read questions carefully to avoid mistakes. | Test forms with actual patients to ensure they are easy to navigate and understand. Use large, legible fonts. | The patient experience is positive and less stressful, leading to higher completion rates and better quality information. |
By working together, patients and providers can transform the intake process from a tedious task into a valuable tool for effective care. When patients arrive prepared and providers offer well-designed forms, the foundation is set for a productive and successful medical appointment.
Your Action Plan for Intake Excellence
Improving the healthcare journey starts with refining the medical intake form process, and you have more influence than you might realize. Whether you're a patient or a provider, you can take simple, direct steps to make this crucial first interaction better for everyone.
For Patients: Be a Proactive Partner in Your Care
You can be an advocate for more efficient systems. At your next appointment, ask the office staff if they have a digital option you can fill out ahead of time. A simple question like this can encourage a practice to consider modernizing its process.
To make any appointment smoother, it helps to be prepared. Before you go, gather your:
- Complete medical history
- A list of current medications and their dosages
- Up-to-date insurance information
Having this information ready makes completing any form, whether it's on paper or a tablet, much quicker and ensures your records are accurate.
For Healthcare Teams: Build a Patient-Friendly System
The goal is to adopt systems that make life easier for patients and staff alike. When looking at digital form solutions, prioritize those that connect with your existing EMR. This integration is key to cutting down on the manual data entry that consumes your staff's valuable time.
A gradual rollout can ease the transition. Start with a single department or a specific type of appointment to test the new system and collect feedback. This approach allows you to work out any kinks before a practice-wide launch. By taking these manageable steps, both patients and providers can help create an effective intake system that sets a positive tone for the entire care experience.
Ready to automate your patient intake and scheduling? Learn how Simbie AI can reduce administrative overhead and enhance patient satisfaction for your practice.