For small medical practices, efficient billing is the lifeblood of financial health. Yet, managing claims, patient payments, and revenue cycles can be a monumental task that diverts precious time away from patient care. The right medical billing software for small practices doesn't just automate tasks; it optimizes your entire revenue cycle, reduces claim denials, and ensures you get paid faster. This financial stability is the bedrock upon which quality patient care is built, allowing clinicians to focus on outcomes rather than administrative overhead.
This guide is designed to cut through the noise and provide a clear, comprehensive analysis of the top medical billing solutions on the market. We will review the top medical billing solutions, providing a clear breakdown of their strengths, weaknesses, unique features, and pricing structures. Understanding the broader business process automation benefits for finance can further highlight the value of adopting dedicated software, but our focus here is on practical application for your clinic. In an increasingly complex healthcare landscape, leveraging technology is no longer optional—it's essential for survival and growth.
By the end of this article, you will have a clear understanding of what each platform offers, empowering you to make an informed decision for your practice's financial stability. We provide direct links and screenshots for each tool, so you can see exactly how they work. This comprehensive review will help you select a system that allows you to thrive financially while maintaining a primary focus on what matters most: your patients.
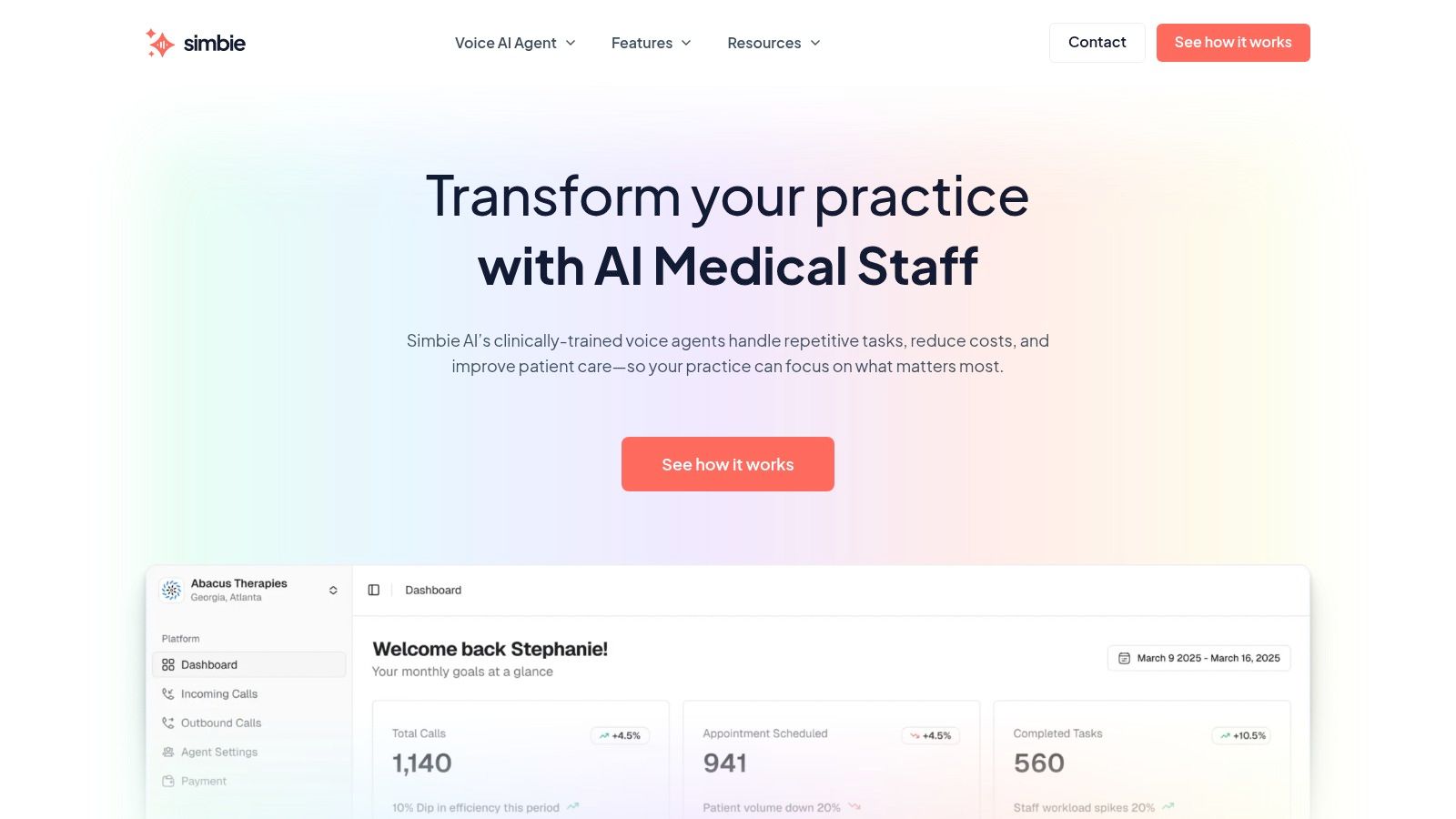
1. Simbie AI: Automating the Front End of Your Revenue Cycle
Simbie AI distinguishes itself in the crowded field of medical billing software for small practices by taking a proactive, preventative approach. Instead of focusing solely on claim submission and reimbursement, Simbie tackles the root cause of most billing errors: inaccurate front-end data. This innovative platform uses a voice-based AI to automate the administrative tasks that precede billing, such as patient intake, scheduling, and crucially, prior authorizations. For small practices, where staff often wear multiple hats, this level of automation is transformative, freeing up valuable human resources for patient-facing activities.
By ensuring pristine data capture from the very first patient interaction, Simbie AI effectively functions as a gatekeeper for your revenue cycle. It cleans up the data pipeline before it flows into your billing system, dramatically reducing the risk of claim denials caused by simple data entry mistakes, incorrect insurance details, or missing authorizations. For a small practice, this translates to less time spent on rework, fewer administrative burdens, and a healthier, more predictable cash flow. It shifts the paradigm from reactive denial management to proactive denial prevention.
Key Features and Strengths
Simbie AI's power lies in its ability to offload critical but repetitive tasks from your front-office staff, allowing them to focus on higher-value patient engagement and complex problem-solving.
- 24/7 AI Voice Agents: Clinically-trained AI agents are available around the clock to handle patient calls. This ensures your practice never misses an appointment request or patient inquiry, capturing revenue opportunities that might otherwise be lost outside of business hours. It also enhances patient access and satisfaction.
- Seamless EMR Integration: The platform integrates directly with your existing Electronic Medical Record (EMR) system. It automatically populates patient charts, reconciles medications, and updates demographic information, eliminating redundant manual data entry and the associated risk of human error. This deep integration is key to its effectiveness.
- Real-Time Eligibility & Authorization: Simbie's AI can verify a patient's insurance eligibility and handle prior authorizations during the initial call. This front-end diligence is a cornerstone of clean claim creation and prevents costly denials down the line, directly impacting the practice's bottom line.
- Proven ROI: The platform has demonstrated the ability to reduce administrative overhead by up to 60%. This significant cost savings helps alleviate staff burnout and boosts the practice's overall financial health, making it a strategically sound investment.
Practical Implementation
Imagine a new patient calls your practice after hours. Instead of reaching a voicemail, they interact with Simbie's AI agent. The agent collects all necessary demographic and insurance information, verifies their eligibility in real-time, and schedules their first appointment directly in your EMR's calendar. All this happens without any human intervention, creating a complete and accurate patient record ready for the billing process the moment the patient walks in the door. This efficiency extends to existing patients needing to reschedule or confirm appointments, reducing phone tag and administrative friction.
Pros and Cons
| Pros | Cons |
|---|---|
| 24/7 Availability: AI agents ensure no missed calls and continuous patient support, maximizing appointment booking. | Utilization-Based Cost: Pricing model may require small practices to monitor usage to ensure a positive return. |
| Reduces Administrative Burden: Automates routine tasks, leading to significant cost savings and reduced staff burnout. | Limited Scope: Highly complex clinical queries or nuanced patient situations may still need to be escalated to staff. |
| Improves Data Accuracy: Catches errors at the source, leading to a much higher clean claim rate. | |
| Scalable & Secure: The HIPAA-compliant platform grows with your practice and includes manual overrides for safety. |
Website: https://www.simbie.ai
2. Tebra (Kareo Billing)
Tebra, which absorbed the well-known Kareo Billing platform, offers a robust, cloud-based solution designed from the ground up for independent and small medical practices. It streamlines the entire billing workflow, from verifying patient eligibility to processing payments, making it a powerful contender for practices looking to simplify their financial operations. The platform's core strength lies in its dedicated focus on the needs of smaller organizations that require efficiency without a massive IT footprint or a dedicated team of billing specialists.
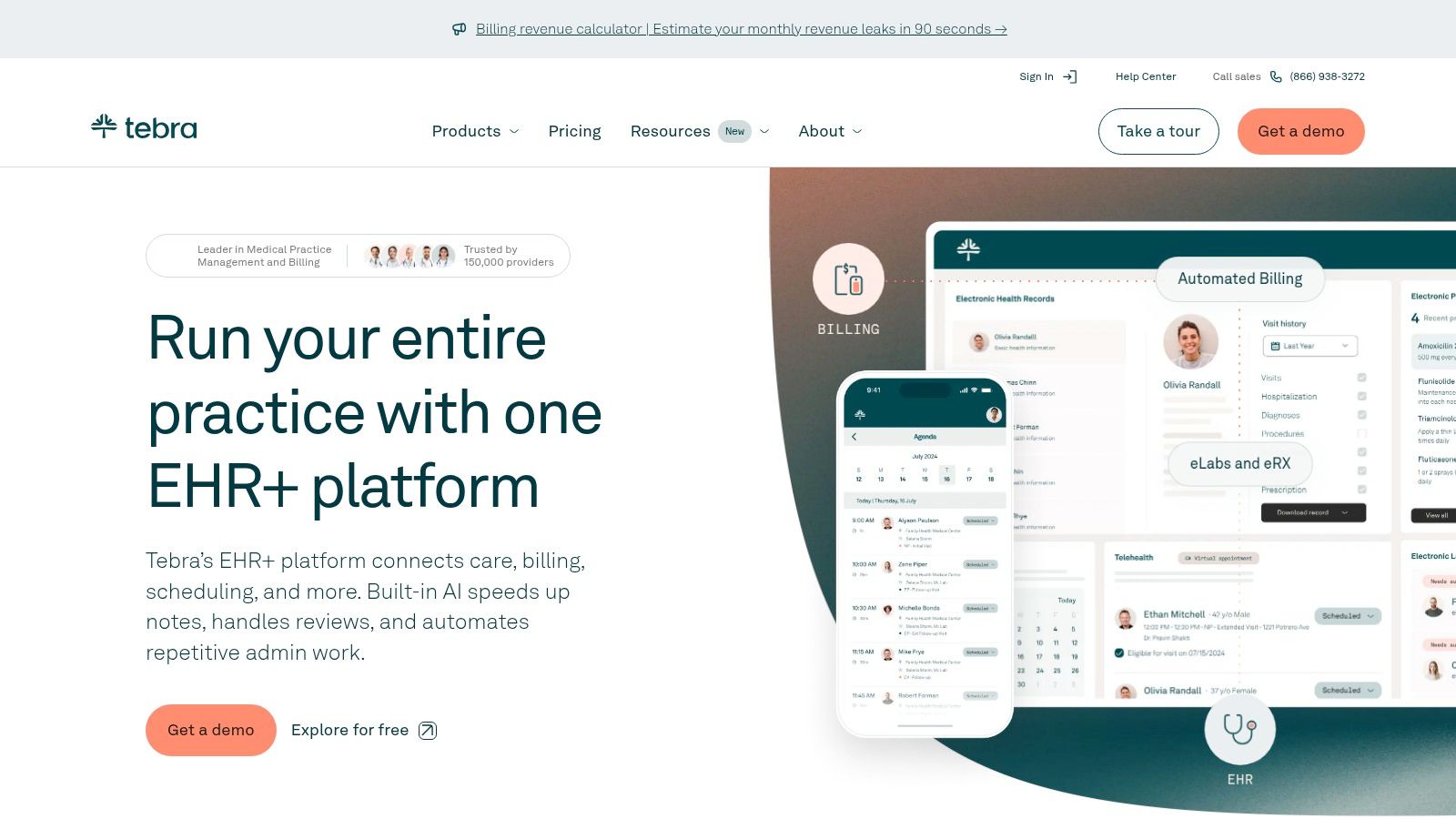
Tebra stands out by combining comprehensive billing features with a user-friendly interface that doesn't require extensive training to master. This makes it an excellent choice for medical billing software for small practices that may not have dedicated billing experts on staff. The system supports a massive network of over 4,000 government and commercial payers, ensuring broad compatibility for claim submissions. Its dashboard-driven approach provides at-a-glance visibility into key performance indicators (KPIs) like days in A/R and claim rejection rates, empowering practice managers to make data-driven decisions.
Key Features & Benefits
Tebra’s platform is built to handle the most critical aspects of the billing cycle with precision and ease. Key functionalities include:
- Comprehensive Claim Management: The software includes an advanced claim scrubber that automatically checks for errors against a vast library of payer rules before submission, significantly reducing denial rates. It supports both CMS-1500 and ANSI 837 claim formats and provides clear, actionable feedback on rejected claims.
- Integrated Patient Payments: Tebra Payments allows practices to accept patient credit, debit, and FSA/HSA cards with transparent, flat-rate processing fees. This simplifies collecting patient responsibilities and integrates seamlessly with the patient ledger, reducing manual reconciliation efforts.
- Eligibility Verification: Real-time eligibility checks help prevent claim denials by confirming patient coverage details, copays, and deductibles upfront. This saves administrative time, reduces billing errors, and improves the patient financial experience by providing clarity on their responsibility.
- Automation Add-Ons: For practices looking to further boost efficiency, Tebra offers optional Robotic Process Automation (RPA) tools to automate repetitive tasks like data entry and payment posting. This allows staff to focus on more complex, high-value activities like denial follow-up.
Pro Tip: When setting up Tebra, take advantage of the claim scrubbing rules editor. Customize it to flag common coding errors specific to your specialty. This small step can dramatically improve your first-pass claim acceptance rate.
Pricing and Implementation
Tebra uses a per-provider, per-month subscription model, though you must contact them for a custom quote. This structure allows the software to scale with your practice's growth. The cloud-based setup is quick, typically requiring minimal IT involvement. However, since features are split across modules (Billing, Clinical EHR, Patient Experience), be sure to clarify which bundle best fits your needs to avoid unexpected costs. Understanding these components is crucial for optimizing your revenue cycle with this platform. For a deeper dive into financial best practices, explore these strategies for healthcare revenue cycle optimization.
Website: https://www.tebra.com
3. AdvancedMD
AdvancedMD offers a comprehensive, cloud-based suite that unifies practice management, EHR, and medical billing into a single ecosystem. Its modular approach is particularly well-suited for independent practices that want to build a custom solution, starting with billing and adding other functions as they grow. This platform is designed to scale, accommodating solo practitioners and expanding multi-provider groups with equal efficiency, making it a long-term strategic partner rather than just a software purchase.
What makes AdvancedMD a strong choice for medical billing software for small practices is its unique blend of robust features and customizable packaging. Practices can choose software-only solutions, full revenue cycle management (RCM) services, or a hybrid of both. This flexibility allows a practice to start by managing billing in-house and later transition to outsourcing as patient volume increases, all within the same platform. Its transparent online pricing configurator allows you to build a bundle and get an initial estimate, a rarity in the industry that empowers buyers.
Key Features & Benefits
AdvancedMD is engineered to streamline financial workflows and provide deep operational insights through powerful analytics. Key functionalities include:
- Customizable Bundles: Practices can select from à la carte tools or pre-packaged bundles that include practice management, EHR, telehealth, and billing, ensuring you only pay for what you need. This avoids the bloat and expense of features irrelevant to your practice.
- Intelligent Claim Scrubber: The ClaimInspector tool provides built-in edits and automatically scrubs claims for errors before submission, boosting first-pass acceptance rates and accelerating reimbursements. It checks against both general and payer-specific rules.
- Specialty-Specific Editions: The software offers tailored editions for various specialties, including mental health, physical therapy, and more, with customized templates, workflows, and billing codes. This specialization reduces the need for extensive customization post-purchase.
- Automated Payment Posting: The platform supports automatic posting of Electronic Remittance Advice (ERAs), which drastically reduces manual data entry and potential errors. This feature alone can save a small practice hours of administrative work each week.
Pro Tip: Use the online pricing configurator to experiment with different bundles. This will give you a clear baseline budget before scheduling a sales demo, empowering you to negotiate a package that perfectly fits your practice's needs and financial constraints.
Pricing and Implementation
AdvancedMD uses a quote-based, per-provider, per-month pricing model, but its online configurator provides a transparent starting point. Discounts are often available for multi-provider practices and bundled service commitments. While the platform is powerful, its comprehensive nature means implementation can be more involved than simpler systems, often requiring dedicated training sessions. If you're looking for an all-in-one solution, it’s worth understanding which practice management software features are most critical to your operations to ensure the bundle you choose provides maximum value.
Website: https://www.advancedmd.com/plans-pricing/
4. DrChrono (by EverHealth)
DrChrono, now part of EverHealth, provides an integrated EHR and practice management platform with robust billing capabilities tailored for modern, often mobile, small practices. It’s designed as an all-in-one system, aiming to unify clinical and financial workflows from appointment scheduling to final payment. The platform's strength is its mobile-first approach, particularly its optimization for iPad and iPhone, which allows providers and staff to manage billing tasks, approve charges, and view patient accounts on the go, untethering them from a desk.
DrChrono earns its spot by offering a flexible growth path. Small practices can start with its powerful in-house billing tools and later add on its managed Revenue Cycle Management (RCM) services as their needs evolve. This scalability makes it an excellent choice of medical billing software for small practices that anticipate growth but want to maintain control over their initial billing processes without committing to a full-service RCM solution upfront. The ability to seamlessly switch between in-house and outsourced billing within one system is a significant advantage.
Key Features & Benefits
DrChrono’s platform integrates billing directly into the clinical workflow to reduce manual data entry and errors at the point of care. Key functionalities include:
- Automated Claim Generation: The system automatically creates CMS-1500 and 837 claim forms using data from billing and appointment profiles, which streamlines the submission process. Charges captured during the clinical encounter flow directly to the billing module, minimizing revenue leakage.
- Integrated Patient Payments: DrChrono offers multiple ways to collect patient payments, including card-on-file, online payments through a patient portal, and modern text-to-pay options, with clearly published processing rates for financial transparency.
- Flexible RCM Services: Practices have the option to outsource their entire billing process to DrChrono’s team of experts. This provides a seamless transition if in-house billing becomes too burdensome, allowing the practice to leverage professional billers familiar with the software.
- Mobile-Centric Workflow: The entire platform is optimized for iOS, allowing practitioners to manage billing tasks, view patient ledgers, and process payments directly from an iPad or iPhone. This is ideal for physicians who move between exam rooms or work from multiple locations.
Pro Tip: Use DrChrono's appointment profiles to pre-load common billing codes for specific visit types. This automates charge capture during the encounter, ensuring no services are missed and claims are generated accurately and instantly.
Pricing and Implementation
DrChrono's software plan pricing is available by quote, so you'll need to contact their sales team for specific details. While some fees apply for paper claims and statements, they offer transparent, flat-rate pricing for their integrated payment processing. User reviews sometimes note a learning curve for advanced features and variable customer support experiences, so a thorough demo is recommended. The platform’s strength lies in its ability to support your practice as it grows, making a full understanding of its EHR capabilities a key step. To learn more about this, explore these strategies for electronic health record optimization.
Website: https://www.drchrono.com
5. CollaborateMD (a Waystar company)
CollaborateMD, now part of the Waystar family, delivers a cloud-based medical billing and practice management solution tailored for efficiency and transparency. It serves both in-house billing teams and third-party billing companies, offering a scalable platform that emphasizes clean claim submission from the start. The system is particularly appealing for smaller or newer practices due to its clear, published pricing and relentless focus on maximizing first-pass acceptance rates, which is a critical factor for maintaining healthy cash flow.
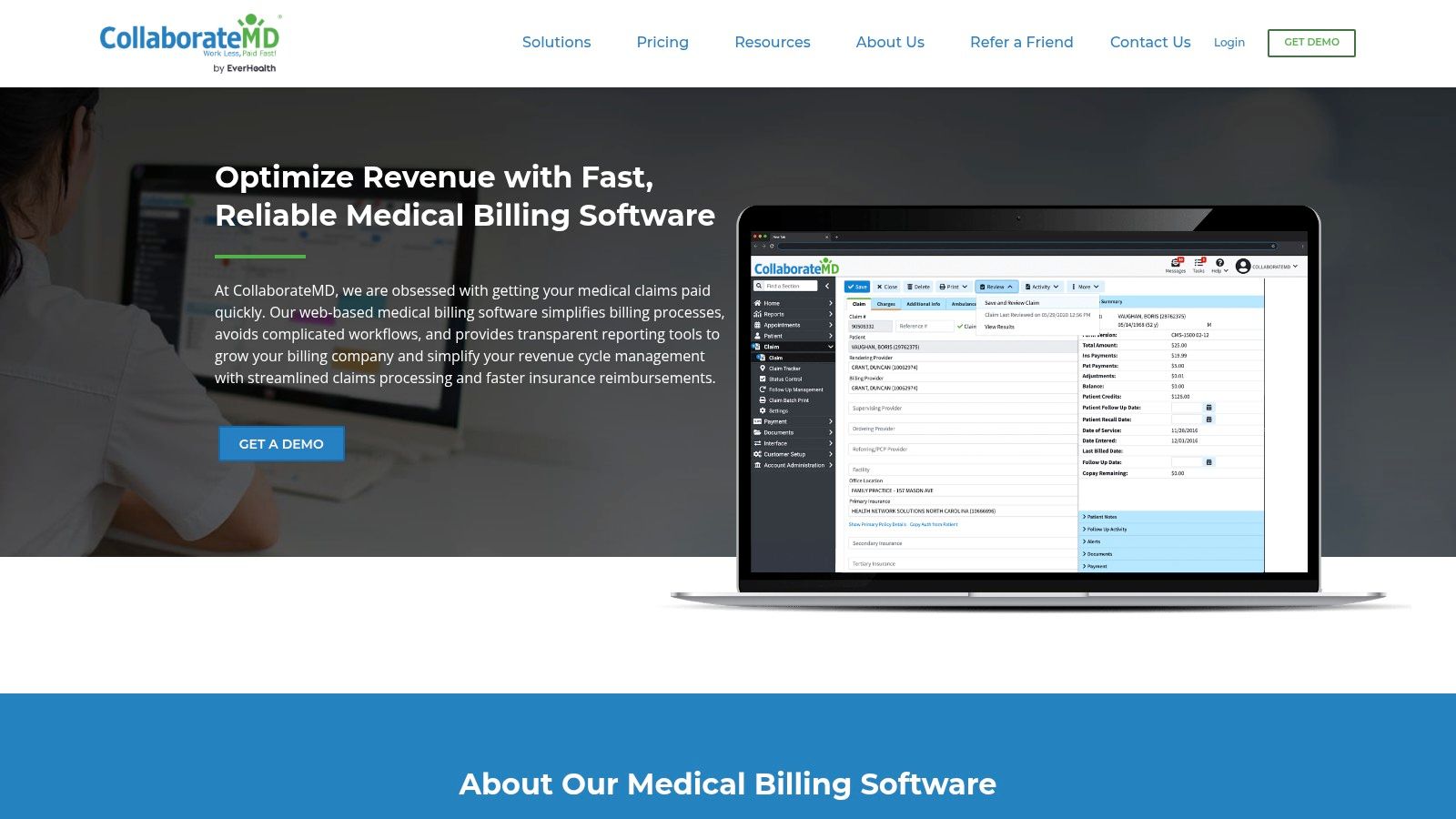
What makes CollaborateMD a strong choice for medical billing software for small practices is its dedication to minimizing claim errors through powerful, built-in edits and real-time feedback. Its real-time claim submission and tracking capabilities provide immediate feedback from payers, allowing billers to correct issues on the spot rather than waiting days for rejections to come back. This proactive approach to revenue cycle management helps maintain a steady cash flow, a critical factor for independent providers who cannot afford long payment cycles.
Key Features & Benefits
CollaborateMD is designed to simplify complex billing workflows with powerful, user-friendly tools that deliver measurable results. Its key functionalities include:
- Real-Time Claim Scrubber: The platform features a robust claims scrubber with Level-2 edits, which checks claims against a vast database of payer rules in real time, dramatically increasing the likelihood of clean claim submissions. This is more advanced than simple batch scrubbing.
- Comprehensive Claim Tracking: Users can monitor the entire lifecycle of a claim from creation to final payment within a single dashboard, providing complete visibility and control over accounts receivable. Alerts can be set for aging or un-responded claims.
- Automated ERA Posting: The system automatically posts Electronic Remittance Advice (ERA), significantly reducing the manual effort required for payment reconciliation and allowing staff to focus on exceptions and denials rather than routine data entry.
- Detailed Analytics and Reporting: Powerful dashboards provide at-a-glance insights into financial performance, helping practices identify trends, pinpoint revenue leaks, and make data-driven decisions. Reports can be customized to track key metrics specific to the practice's specialty.
Pro Tip: Utilize CollaborateMD’s detailed rejection and denial management reports to identify recurring error patterns. Isolating the root cause of common issues, such as incorrect modifier usage or eligibility problems, can lead to systemic improvements in your billing process.
Pricing and Implementation
CollaborateMD stands out with its transparent, publicly available pricing. It offers tiered, per-provider fees with a monthly minimum, making it an affordable entry point for low-volume practices. However, be aware of potential extra charges for additional tax IDs or specific transaction types. As a cloud-based solution, implementation is straightforward and does not require significant IT resources. While it interfaces with many EHRs, it's primarily a billing and practice management system, so practices needing an all-in-one clinical and financial solution may need to integrate it with a separate EHR.
Website: https://www.collaboratemd.com/solutions/medical-billing-software/
6. PracticeSuite
PracticeSuite offers a flexible, cloud-based platform that combines medical billing, practice management, and EHR capabilities into one scalable solution. It is specifically designed for small or low-volume practices that need affordability without sacrificing core functionality. The platform's modular approach allows users to start with standalone billing software and expand to a full suite as their needs grow, providing a clear and cost-effective upgrade path. This makes it an ideal starting point for new practices.
What makes PracticeSuite a strong choice is its unique blend of do-it-yourself software with optional managed billing services. This hybrid model makes it an excellent medical billing software for small practices that may want to handle billing in-house initially but have the option to outsource to the same vendor later. This flexibility ensures practices can adapt their revenue cycle strategy without the disruption and cost of migrating to a new system. It provides a safety net for practices that may find their billing needs outgrow their internal capacity.
Key Features & Benefits
PracticeSuite is built to provide essential tools for efficient revenue cycle management while remaining accessible for smaller teams. Key features include:
- Flexible Claim Management: The system includes a robust claims engine with features like batch eligibility checks, electronic remittance advice (ERA) auto-posting, and detailed aging reports to track unpaid claims. Its workflow tools help organize follow-up tasks for billers.
- Scalable Platform Tiers: Practices can choose from standalone Practice Management, a combined PM/Billing solution, or the complete EHR and RCM suite, allowing for customized deployment. This prevents practices from overpaying for unused features.
- Integrated RCM Services: For practices that need more support, PracticeSuite offers outsourced revenue cycle management (RCM) services, providing expert billing support directly within the platform. This ensures consistency and leverages the expertise of professionals who know the software inside and out.
- Comprehensive Reporting: The software provides a wide array of financial reports, dashboards, and key performance indicators to give practice managers clear visibility into their financial health, collection rates, and denial trends.
Pro Tip: If you're starting with the basic billing plan, utilize the platform's detailed A/R aging reports from day one. Set a recurring weekly task to review claims over 30 days old to proactively address potential payment delays and keep your cash flow healthy.
Pricing and Implementation
PracticeSuite is known for its transparent pricing, often promoting affordable starting rates for its billing and practice management modules. However, the final cost is based on a custom quote that depends on the specific modules selected, the number of providers, and claim volume. Its cloud-based nature ensures a quick setup process with minimal technical overhead. When requesting a quote, be sure to clarify which features are included in each plan tier to ensure you select the package that best supports your practice's billing workflow and avoids future surprise costs.
Website: https://practicesuite.com/pricing
7. Capterra’s Medical Billing Software Category
Instead of a single software solution, Capterra is an invaluable research platform that functions as a comprehensive online marketplace for business software. For a small practice navigating a crowded market, Capterra’s dedicated medical billing software category serves as a crucial starting point. It allows decision-makers to compare dozens of vendors side-by-side, filter options based on specific needs, and read verified user reviews to gauge real-world performance. This makes it an essential tool for due diligence before committing to a platform and helps avoid costly mistakes.
Capterra stands out by empowering small practices with the data needed to make an informed choice. Its transparent, user-driven approach helps cut through marketing jargon, providing a clearer picture of a software’s strengths and weaknesses. This is particularly useful when looking for medical billing software for small practices, as the platform allows you to filter specifically for vendors that cater to your practice size, specialty, and deployment preference (cloud-based vs. on-premise). It transforms a potentially overwhelming research process into a structured, manageable task.
Key Features & Benefits
Capterra's value lies in its powerful research and comparison tools designed to simplify the selection process and build confidence in your final choice. Key functionalities include:
- Side-by-Side Vendor Comparison: Users can select multiple software options and compare them on a detailed grid covering features, pricing models, and user ratings. This provides a direct, at-a-glance overview of top contenders, highlighting key differentiators.
- Verified User Reviews: The platform hosts thousands of reviews from authenticated users, complete with pros and cons, which offer authentic insights into a product's usability, customer support, and overall value. These unfiltered opinions are often more valuable than a sales demo.
- Advanced Filtering Options: You can narrow the vast list of software by features (like claim scrubbing or patient portals), practice size (e.g., 1-10 physicians), and pricing structure, ensuring you only see relevant solutions that meet your core requirements.
- Up-to-Date Buyer Guides: Capterra provides articles and guides that break down industry trends, pricing, and key considerations, educating buyers throughout their journey. This content helps you ask the right questions during vendor demos.
Pro Tip: Use Capterra’s comparison tool to create a shortlist of 3-5 top-rated vendors. Then, read the most recent one- and two-star reviews for each. This will reveal recurring issues or potential deal-breakers that glowing reviews might overlook.
Pricing and Implementation
Access to Capterra’s comparison tools, reviews, and guides is completely free for software buyers. The platform makes money through vendor referral fees and sponsored listings. While pricing information on individual software pages is provided, it is vendor-submitted and often requires contacting the vendor directly for an accurate quote. The main implementation step here is using the platform effectively to build a shortlist before scheduling demos with your top choices. Be aware that sponsored listings may appear higher in search results, so always sort by "Highest Rated" to get an unbiased view.
Website: https://www.capterra.com/medical-billing-software/
Medical Billing Software Comparison: Top 7 Solutions
| Product | Implementation Complexity 🔄 | Resource Requirements ⚡ | Expected Outcomes 📊 | Ideal Use Cases 💡 | Key Advantages ⭐ |
|---|---|---|---|---|---|
| Simbie AI | Medium – AI integration & setup | Moderate – EMR integration | Up to 60% admin cost savings, zero missed calls | Healthcare practices focusing on admin automation | 24/7 voice agents, seamless EMR integration, HIPAA-compliant |
| Tebra (Kareo Billing) | Low – Cloud-based setup | Low – per provider subscription plus fees | Efficient claims processing and payment handling | Small, independent practices needing billing | Broad payer network, RPA automation option, clear transaction pricing |
| AdvancedMD | Medium-High – Modular customization | Medium-High – multiple modules and bundles | Scalable billing and practice management solutions | Practices needing integrated EHR + billing | Transparent configurator, specialty editions, multi-provider scale |
| DrChrono (by EverHealth) | Medium – mobile-friendly setup | Low to Medium – depends on billing in-house or RCM | Flexible billing growth, mobile optimized workflows | Mobile/small practices starting with in-house billing | Mobile focus, transparent payment rates, optional RCM support |
| CollaborateMD (Waystar) | Low-Medium – cloud with claim edits | Low – transparent pricing with monthly minimums | High clean claim rates, detailed analytics | Low-volume providers and billing companies | Real-time submissions, published pricing, strong analytics dashboards |
| PracticeSuite | Low-Medium – modular selection | Low to Medium – scalable plans | Flexible scalable billing and practice management | Small or low-volume practices expanding services | Affordable starting rates, user positive feedback, optional RCM |
| Capterra’s Medical Billing Software Category | Very low – marketplace tool | Minimal – online access and filtering | Streamlined software vendor vetting and decision-making | Any practice evaluating billing options | Verified user reviews, broad vendor coverage, buyer guides |
Making the Right Choice for Your Practice's Financial Future
Selecting the right medical billing software for small practices is more than just an operational upgrade; it's a foundational business decision. Your choice directly impacts cash flow, administrative efficiency, and the amount of time your team can dedicate to patient care. Throughout this guide, we've explored a range of powerful solutions, each designed to address the unique challenges that small and growing clinics face, from managing complex payer rules to improving patient collections.
From the all-encompassing practice management suites like Tebra (formerly Kareo Billing) and AdvancedMD to the streamlined, user-friendly platforms of CollaborateMD and PracticeSuite, the options are diverse. We've seen how tools like DrChrono integrate billing seamlessly with EHR functionalities, and how innovative AI-driven solutions like Simbie AI are revolutionizing the revenue cycle by automating complex tasks. The key takeaway is that there is no single "best" software, only the one that is best suited for your specific needs, workflow, and long-term strategic goals.
Your Action Plan for Selecting the Right Software
To move from evaluation to implementation, you need a clear, structured plan. Avoid making a decision based on a features list alone. Instead, focus on how a platform will integrate into your daily operations and support your long-term vision. A hasty choice can lead to costly implementation failures and staff frustration.
Here are the actionable next steps to guide your decision-making process:
- Define Your Core Needs: Revisit your initial pain points. Are you struggling with claim denials, slow payment cycles, inefficient patient intake, or a lack of reporting? Create a checklist of "must-have" features versus "nice-to-have" features. This will be your primary filter. For example, if you are a specialty practice, specialty-specific templates might be a "must-have".
- Shortlist Your Top 3 Contenders: Based on our reviews and your needs checklist, narrow down your options to two or three platforms. This manageable number allows for a deep-dive comparison without causing decision fatigue. Use a spreadsheet to track features, pricing, and your impressions of each.
- Schedule Live Demos: This is the most critical step. A live demo allows you to see the software in action and ask role-specific questions. Involve a key member of your billing staff in the demo, as they will be a primary user and can offer invaluable insights into the usability of the interface and the efficiency of the workflow.
- Ask the Tough Questions: During your demos, go beyond the sales pitch. Inquire about the implementation process, data migration support, the average customer support response time, and any hidden fees associated with training, clearinghouses, or add-on modules. Ask for references from practices similar to yours in size and specialty.
Final Considerations for a Successful Implementation
Remember that implementing new medical billing software for small practices is a significant project. Plan for a transition period where your team will need training and time to adapt. A successful rollout depends as much on your implementation strategy as it does on the software itself. Choosing a partner with excellent customer support and a clear onboarding process can make all the difference. Create an internal champion for the new software who can help train others and encourage adoption.
Ultimately, this investment is about securing your practice's financial health and future-proofing your operations. To secure a prosperous financial future, small practices must continually evaluate and implement effective business growth strategies. Choosing the right software is a critical component of that plan, enabling you to optimize revenue, reduce administrative burdens, and focus on what truly matters: delivering exceptional care to your patients.
Ready to eliminate claim denials and automate your revenue cycle with the power of AI? Discover how Simbie AI works with your existing EHR to provide a 99.4% clean claim rate and reduce administrative workload by up to 85%. See how our specialized medical billing software for small practices can transform your financial operations by visiting Simbie AI today.

