Boost Your Bottom Line: Proven Strategies for Practice Growth
Want to increase medical practice revenue? This listicle provides seven actionable strategies to boost your bottom line and improve your practice’s financial health. Learn how to optimize revenue cycle management, integrate telehealth, explore value-based care, and leverage other key tactics to enhance profitability and patient satisfaction. These proven methods will help your practice thrive in the current healthcare environment.
1. Revenue Cycle Management (RCM) Optimization
One of the most impactful strategies to increase medical practice revenue is through Revenue Cycle Management (RCM) optimization. This comprehensive approach focuses on managing the financial processes of your practice, from the moment a patient registers to the final payment collection. By streamlining every step, RCM optimization aims to reduce delays, minimize claim denials, and maximize revenue collection through improved processes, technology, and staff training. In a competitive healthcare landscape, efficient RCM is no longer a luxury, but a necessity for financial stability and growth. This is why it deserves a top spot on our list for increasing medical practice revenue.
RCM optimization works by identifying and addressing bottlenecks in your current revenue cycle. This often involves automating manual tasks, improving communication between different departments (like front desk, billing, and clinical staff), and implementing robust analytics to track performance and identify areas for improvement. Features like automated patient eligibility verification ensure accurate information is captured upfront, reducing the risk of denials later. Real-time claim scrubbing and validation tools catch errors before submission, further minimizing denials and accelerating the payment process. Robust denial management and appeals processing systems help recoup lost revenue, while patient payment portals offer convenient payment options and improve transparency, ultimately enhancing patient satisfaction. Analytics and reporting dashboards provide valuable insights into key performance indicators, enabling data-driven decision-making and continuous improvement. Finally, prior authorization management streamlines the often complex process of obtaining insurance pre-approvals, preventing delays in care and ensuring timely reimbursement.
The benefits of RCM optimization are significant. Studies show that it can reduce claim denial rates by 20-30%, which directly translates to increased revenue. Faster payments improve cash flow, allowing practices to reinvest in their operations and expand services. By automating tasks and streamlining processes, administrative costs are reduced, freeing up staff to focus on patient care. Furthermore, transparent billing practices and convenient payment options lead to enhanced patient satisfaction, building stronger patient-provider relationships and promoting patient loyalty.
Several healthcare organizations have seen substantial success with RCM optimization. The Cleveland Clinic, for example, reduced denial rates from 8% to 3% after implementing a comprehensive RCM strategy. Mercy Health saw a 15% increase in collections within six months of adopting similar measures. These examples demonstrate the tangible impact of RCM optimization on a practice’s financial health.
While the benefits are substantial, it’s crucial to acknowledge the challenges associated with RCM optimization. It requires a significant upfront investment in technology and staff training. Implementing new systems and workflows can be disruptive, and change management can be challenging. Ongoing maintenance and updates are also necessary to ensure the system remains effective and compliant with evolving regulations.
To begin optimizing your revenue cycle, consider these actionable tips:
- Start with denial analysis: Identify the top reasons for claim denials in your practice and target those areas for improvement.
- Implement patient eligibility verification at scheduling: Verify insurance coverage and patient responsibility upfront to avoid surprises later.
- Use automated claim scrubbing before submission: Identify and correct coding errors and other issues that can lead to denials.
- Track key performance indicators: Monitor metrics like days in accounts receivable (A/R) and collection rates to measure the effectiveness of your RCM efforts.
Popular RCM solutions are offered by companies like Epic Systems, Cerner Corporation, athenahealth, and Change Healthcare.
The following infographic visualizes the core steps of revenue cycle management: Eligibility Verification, Claim Scrubbing & Validation, and Payment Collection. This simplified process flow illustrates how optimizing each step can contribute to increased revenue.
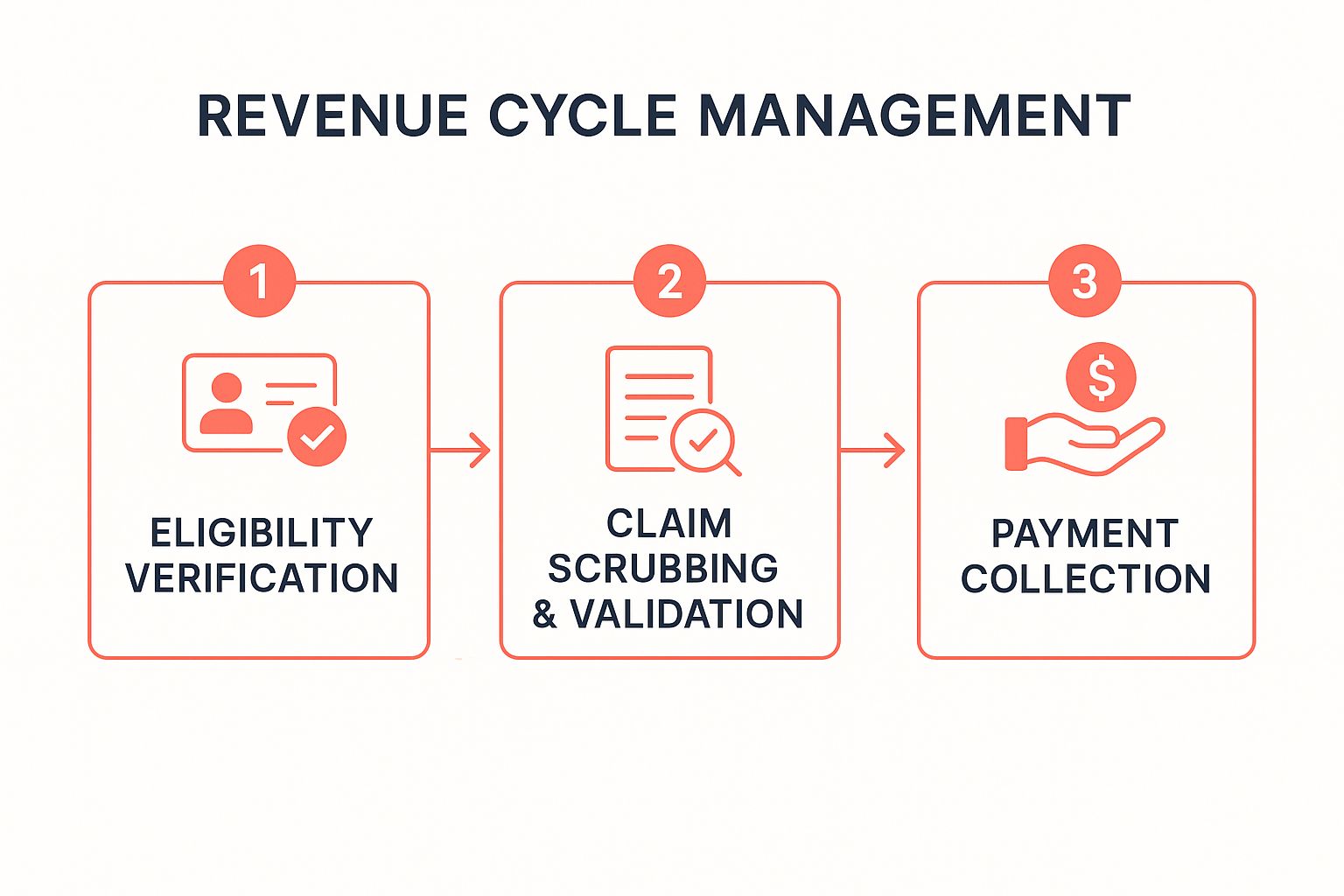
This infographic highlights the interconnectedness of the three core RCM steps. By ensuring accurate eligibility verification upfront, followed by thorough claim scrubbing and validation, practices can significantly improve the efficiency of payment collection and increase overall revenue.
Despite the challenges, the potential benefits of RCM optimization far outweigh the costs. By implementing the strategies and tips outlined above, medical practices of all sizes can streamline their financial processes, reduce denials, improve cash flow, and ultimately, increase revenue, securing their financial stability and enabling them to deliver high-quality patient care.
2. Telemedicine and Virtual Care Services
Telemedicine and virtual care services represent a significant shift in how healthcare is delivered, offering a powerful avenue to increase medical practice revenue. By leveraging digital platforms, practices can expand their reach, reduce overhead, and offer convenient care options that resonate with today’s patients. This strategy encompasses a range of services, from video consultations and remote monitoring to digital prescription management and virtual follow-up appointments, creating new revenue streams while simultaneously enhancing patient access. Integrating telemedicine isn’t just about keeping up with the times; it’s a strategic move to optimize operations and boost your bottom line.

In essence, telemedicine replaces traditional in-person visits with virtual interactions whenever appropriate. Patients can connect with their healthcare providers from the comfort of their homes, eliminating travel time and costs. This is particularly beneficial for routine follow-ups, chronic disease management, and even some initial consultations. Through video conferencing, providers can assess patients, discuss symptoms, adjust medications, and provide education, much like they would in a traditional office setting. Remote patient monitoring tools allow continuous tracking of vital signs and other health data, enabling proactive interventions and reducing the need for frequent in-person visits. This not only increases efficiency but also empowers patients to take a more active role in their healthcare.
The success of telemedicine is well-documented. The Mayo Clinic witnessed a remarkable 50-fold increase in virtual visits during 2020-2021, demonstrating the rapidly growing demand for this type of care. Kaiser Permanente, a leading integrated healthcare system, generated an impressive $2.4 billion in telemedicine revenue in 2021, highlighting the significant financial potential. Even specialized practices, like dermatology, have seen revenue increases of 25-40% through the implementation of teledermatology. These examples underscore the viability and profitability of telemedicine across various medical specialties.
The benefits of incorporating telemedicine into your practice are numerous. It expands your patient base beyond geographical limitations, allowing you to reach individuals who might otherwise lack access to specialized care. No-show rates decrease significantly, as virtual appointments offer greater flexibility and convenience. Lower overhead costs compared to in-person visits contribute directly to increased revenue. Improved patient convenience and satisfaction lead to better retention and positive word-of-mouth referrals. Finally, new service offerings through telemedicine generate additional revenue streams, bolstering the practice’s financial health.
However, it’s crucial to acknowledge the potential challenges. Technology barriers may exist for some patient populations, requiring careful consideration and support. Limited physical examination capabilities necessitate clear guidelines for when virtual care is appropriate. Variations in insurance reimbursement for telehealth services require diligent billing practices. Finally, initial setup and training costs need to be factored into the budget.
To successfully implement telemedicine, consider these actionable tips:
- Start small: Begin with follow-up appointments and consultations to familiarize both staff and patients with the technology and workflow.
- Ensure HIPAA compliance: Choose platforms that adhere to HIPAA regulations to protect patient privacy and security.
- Train your staff: Provide thorough training on virtual care workflows, including using the technology, scheduling appointments, and addressing patient inquiries.
- Market your services: Promote your telemedicine services to existing patients first, highlighting the convenience and benefits.
- Verify insurance coverage: Confirm insurance coverage for telehealth services to ensure proper reimbursement.
Platforms like Teladoc Health, Amwell, Doxy.me, and SimplePractice offer comprehensive solutions for implementing telemedicine, providing features like video consultation platforms, remote patient monitoring capabilities, digital prescription management, virtual follow-up appointment scheduling, mobile health app integration, and cross-platform compatibility.
Integrating telemedicine and virtual care services deserves a prominent place in any strategy to increase medical practice revenue. By understanding the features, benefits, and potential challenges, and by implementing these practical tips, your practice can leverage this powerful tool to optimize care delivery, enhance patient satisfaction, and achieve significant financial growth.
3. Value-Based Care Contracting
Value-based care contracting is a powerful strategy to increase medical practice revenue while simultaneously enhancing the quality of patient care. In the traditional fee-for-service model, practices are reimbursed based on the volume of services they provide. This can incentivize unnecessary tests and procedures. Value-based care flips this model on its head, focusing instead on patient outcomes and rewarding practices for delivering high-quality, cost-effective care. This shift aligns incentives with patient needs and can significantly increase medical practice revenue through performance bonuses and shared savings. This approach is increasingly relevant in today’s healthcare landscape, as payers and patients alike demand better value and improved outcomes.
This model operates by establishing contracts between healthcare providers and payers (like insurance companies or government programs). These contracts define specific quality metrics, patient satisfaction targets, and cost-effectiveness benchmarks that practices must achieve. By meeting or exceeding these targets, practices earn financial incentives. This encourages a proactive approach to care, focusing on prevention, chronic disease management, and care coordination to improve patient health and reduce unnecessary healthcare utilization.
For example, Geisinger Health System’s ProvenCare program, a pioneer in value-based care, has demonstrably increased margins by 7-8% by bundling payments for specific episodes of care and guaranteeing quality outcomes. Similarly, Advocate Health Care achieved $60 million in shared savings through its participation in Accountable Care Organizations (ACOs), demonstrating the financial viability of this model. ChenMed, a primary care provider focused on value-based care for seniors, has reported a 15% increase in revenue per patient through its value-based contracts. These successes highlight how value-based care can drive significant revenue growth while simultaneously improving patient outcomes.
Implementing value-based care contracting requires specific infrastructure and strategic adjustments. Key features include:
- Quality Metric Tracking and Reporting: Robust systems to monitor and report on quality indicators are crucial.
- Patient Outcome Measurement Systems: Tools to accurately assess patient health outcomes and satisfaction levels.
- Cost-Effectiveness Analysis Tools: Methods to track and analyze the cost of care in relation to outcomes.
- Care Coordination Protocols: Establishing clear processes for coordinating care across different providers and settings.
- Population Health Management: Strategies to proactively manage the health of specific patient populations.
- Risk-Sharing Arrangements: Agreements that distribute financial risk and reward between payers and providers.
Value-based care contracting offers numerous advantages for practices looking to increase medical practice revenue:
- Higher Reimbursement Rates for Quality Care: Practices are rewarded for delivering superior care.
- Predictable Revenue Streams: Value-based contracts offer more stable and predictable revenue compared to the volatility of fee-for-service.
- Improved Patient Outcomes and Satisfaction: The focus on quality and coordination leads to better patient experiences.
- Reduced Administrative Burden Over Time: By streamlining care and reducing unnecessary services, administrative tasks can be minimized.
- Competitive Advantage in the Market: As value-based care becomes increasingly prevalent, practices that adopt this model gain a competitive edge.
However, transitioning to value-based care also presents challenges:
- Significant Data Collection and Analysis: Tracking and analyzing performance data requires robust IT infrastructure and expertise.
- Initial Investment in Quality Improvement Infrastructure: Investing in new systems and processes can be costly upfront.
- Financial Risk if Quality Targets Aren’t Met: Practices may face financial penalties if they fail to achieve performance goals.
- Complex Contract Negotiations: Negotiating value-based contracts can be complex and require specialized knowledge.
To successfully implement value-based care and increase medical practice revenue, consider these tips:
- Start with Medicare Shared Savings Program (MSSP): This program provides a structured entry point for practices new to value-based care.
- Invest in Care Coordination and Case Management: These are essential for improving patient outcomes and reducing costs.
- Implement Robust Data Analytics Capabilities: Data analysis is crucial for tracking performance and identifying areas for improvement.
- Focus on Preventive Care and Chronic Disease Management: These areas offer significant opportunities for cost savings and improved outcomes.
- Partner with Experienced Value-Based Care Organizations: Seek guidance and support from organizations with a proven track record.
Value-based care, popularized by organizations like the Centers for Medicare & Medicaid Services (CMS), Geisinger Health System, Kaiser Permanente, and Advocate Health Care, is transforming the healthcare landscape. By embracing this model, medical practices can not only increase medical practice revenue but also deliver better, more patient-centered care, positioning themselves for long-term success in a rapidly evolving healthcare environment.
4. Ancillary Service Integration
Ancillary service integration is a powerful strategy to increase medical practice revenue while simultaneously enhancing patient care. It involves strategically adding complementary healthcare services within your existing practice, creating additional revenue streams and offering a more comprehensive, convenient experience for your patients. These services can range from in-house laboratory testing and imaging to physical therapy, pharmacy services, and even aesthetic treatments. By offering these services under one roof, or through strategic partnerships, you can transform your practice into a one-stop shop for patient needs, boosting revenue and patient satisfaction.

This approach works by capitalizing on existing patient traffic and expanding the services available to them. Instead of referring patients out for common tests or procedures, you can perform them in-house, capturing revenue that would otherwise be lost to external providers. This not only increases revenue per patient visit but also improves patient convenience, leading to higher satisfaction and loyalty. Moreover, ancillary services often carry higher profit margins than traditional medical consultations, contributing significantly to your bottom line.
Several successful implementations demonstrate the potential of ancillary service integration to increase medical practice revenue. Family medicine practices that have incorporated in-house laboratory services have reported revenue increases of 15-20%. Dermatology practices offering cosmetic procedures alongside traditional dermatological care have seen a 30-50% boost in revenue per patient. Similarly, orthopedic practices integrating in-house physical therapy have experienced margin increases of up to 25%. These examples highlight how effectively ancillary services can enhance revenue across various medical specialties. Organizations like One Medical, CVS MinuteClinics, Walgreens Healthcare Clinics, and VillageCare have popularized this integrated model, demonstrating its viability and scalability.
Ancillary service integration is particularly beneficial for practices looking to diversify their revenue streams, improve patient retention, and enhance their competitive edge. It’s especially relevant in today’s healthcare landscape, where patients are increasingly seeking convenient, comprehensive care options. This approach also reduces patient “leakage,” where patients are referred out and potentially lost to other providers. By keeping patients within your network for a wider range of services, you strengthen patient relationships and increase lifetime value.
However, integrating ancillary services also comes with challenges. Significant capital investment may be required for equipment, facility modifications, and specialized staff. You’ll also need to navigate additional licensing and regulatory requirements, ensuring compliance with all applicable laws and guidelines. Training existing staff or hiring specialized personnel will be essential for delivering high-quality services. Carefully weigh these factors against the potential benefits before implementing this strategy.
Actionable Tips for Successful Ancillary Service Integration:
- Analyze Referral Patterns: Identify the services your patients are most frequently referred out for. This data will help you pinpoint high-demand services that could be profitably integrated into your practice.
- Start Small and Strategic: Begin with high-volume, low-complexity services that require minimal initial investment and have a lower regulatory burden. This allows you to gain experience and build momentum before expanding to more complex offerings.
- Ensure Proper Licensing and Credentialing: Thoroughly research and comply with all licensing and credentialing requirements for the services you plan to offer. This is crucial for maintaining legal compliance and ensuring patient safety.
- Invest in Training and Staffing: Train your existing staff or hire specialized professionals to deliver the new services. Adequate training is vital for maintaining quality and maximizing the return on your investment.
- Market Your New Services: Effectively communicate the availability of new services to your existing patient base. Use targeted marketing strategies like email campaigns, website updates, and in-office promotions to increase awareness and drive adoption.
Ancillary service integration can be a game-changer for medical practices seeking to increase revenue and enhance patient care. By thoughtfully selecting and implementing complementary services, you can create a more robust and profitable practice while simultaneously providing a more convenient and comprehensive experience for your patients. By carefully considering the pros and cons and following the tips outlined above, you can successfully navigate the complexities of ancillary service integration and reap the significant rewards it offers.
5. Patient Self-Pay and Direct Pay Programs
Are you looking for ways to increase medical practice revenue while simplifying your billing process and fostering stronger patient relationships? Patient self-pay and direct pay programs offer a compelling alternative to traditional insurance-based models, allowing you to bypass the complexities of insurance billing and offer transparent, upfront pricing for services. This approach can significantly improve profit margins, reduce administrative overhead, and provide affordable care options for patients. This model is gaining traction as a viable strategy to increase medical practice revenue, and it deserves serious consideration.
How Direct Pay Works:
Direct pay healthcare delivery models cut out the insurance middleman. Patients pay directly for services, either on a per-visit basis or through a membership model. This allows for transparent pricing structures where patients know exactly what they’re paying for upfront. Several variations exist within this model:
- Membership-based Practices: Patients pay a recurring monthly or annual fee for a defined set of services. This provides predictable revenue streams for the practice and consistent access to care for patients.
- Cash-Only Services: Practices charge a set fee for each service provided, payable at the time of service. This simplifies billing and eliminates the need for claims processing.
- Transparent Pricing Models: Even practices that accept insurance can benefit from transparent pricing by offering clear, upfront pricing for self-pay patients. This empowers patients to make informed decisions about their care and can attract a segment of the population seeking affordable options.
Success Stories:
Several practices have successfully implemented direct pay models and seen significant improvements in their revenue and operations. For example, Atlas MD, a direct primary care (DPC) practice, reportedly generates $8,000-10,000 in monthly revenue per 600 patients, demonstrating the financial viability of this model. The Surgery Center of Oklahoma’s transparent pricing strategy, while not exclusively direct pay, led to a 40% increase in volume by empowering patients with clear cost information. While Qliance, a DPC network, ultimately closed, it demonstrated significant cost savings for patients, averaging around 20%, further highlighting the potential of direct pay to offer affordable care.
Actionable Tips for Implementation:
- Research Local Market Demand: Before transitioning to a direct pay model, thoroughly research the local market to gauge the demand for cash-pay services. Understand the demographics and the willingness of potential patients to pay directly for healthcare.
- Develop Clear, Competitive Pricing: Establish transparent and competitive pricing structures that are easy for patients to understand. Consider offering different membership tiers or package deals to cater to varying needs and budgets.
- Create Attractive Membership Packages: If implementing a membership model, design attractive packages that offer value to patients. Include a clear list of included services, benefits, and any limitations.
- Market the Convenience and Cost Savings: Highlight the convenience and cost savings associated with direct pay in your marketing efforts. Emphasize the simplified billing process, reduced paperwork, and the potential for lower overall healthcare costs.
- Maintain Some Insurance Billing (Optional): For practices transitioning to direct pay, consider maintaining some level of insurance billing for complex procedures or specialist referrals to cater to a broader patient base.
Pros and Cons:
Pros:
- Higher Profit Margins: Eliminating insurance overhead can significantly increase profit margins.
- Predictable Revenue Streams: Membership models provide predictable monthly revenue.
- Reduced Administrative Costs: Simplified billing reduces administrative complexity and costs.
- Faster Payment Collection: Direct payment eliminates the delays associated with insurance claims processing.
- Enhanced Doctor-Patient Relationships: Direct pay models can foster stronger doctor-patient relationships due to increased transparency and direct communication.
Cons:
- Limited Patient Population: Not all patients can afford to pay cash for healthcare services, potentially limiting your patient volume.
- Potential Reduction in Patient Volume: Transitioning to a direct pay model may initially lead to a decrease in patient volume as you adapt to a new patient base.
- Marketing Challenges: Attracting self-pay patients requires targeted marketing efforts to educate potential patients about the benefits of direct pay.
- May Not Cover All Medical Services: Direct pay models may not be suitable for all types of medical services, particularly complex or expensive procedures.
When and Why to Use This Approach:
Direct pay models are particularly well-suited for primary care practices, concierge medicine, and practices offering specialized services with a defined scope. If you’re looking to increase medical practice revenue, simplify your billing process, and cultivate stronger patient relationships, direct pay programs offer a compelling alternative to traditional insurance-based models. While challenges exist, careful planning, targeted marketing, and a focus on patient value can make direct pay a successful strategy to increase medical practice revenue.
6. Advanced Practice Provider (APP) Integration
Integrating Advanced Practice Providers (APPs), such as Nurse Practitioners (NPs) and Physician Assistants (PAs), into your medical practice offers a powerful strategy to increase medical practice revenue while simultaneously enhancing patient care and improving physician satisfaction. This approach allows for expanded service capacity without the significant overhead associated with hiring additional physicians, making it a particularly attractive option for practices looking to boost revenue and improve efficiency. APPs can handle a wide range of responsibilities, freeing up physicians to focus on more complex cases and ultimately increasing the overall patient volume and revenue generation potential of the practice.
APPs are highly trained medical professionals who can conduct physical exams, diagnose and treat illnesses, order and interpret tests, prescribe medications, and counsel patients on preventative care. By strategically integrating APPs into your workflow, you can optimize resource allocation, ensuring that physicians are utilized for their specialized expertise while routine and follow-up appointments are managed efficiently by APPs. This collaborative approach not only increases the number of patients a practice can see but also improves patient access to timely care, a crucial factor in patient satisfaction and retention.
The implementation of APP integration involves several key components. First and foremost, establishing clear collaborative practice agreements that define the scope of each APP’s responsibilities within the legal framework of your state’s regulations is essential. These agreements outline the level of physician supervision required and ensure that APPs practice within their defined scope. Secondly, a robust supervision and mentorship program should be in place to support APPs and facilitate ongoing professional development. This ensures quality of care and allows APPs to grow their skills within the practice. Finally, specialized roles and responsibilities for APPs should be clearly defined, aligning with the practice’s specific needs and the individual APP’s expertise. This might involve assigning APPs to specific departments, patient populations, or types of procedures. Efficient billing and coding processes specific to APP services are also critical to maximize revenue capture.
Several successful examples demonstrate the positive impact of APP integration on revenue and patient care. TeamHealth, a national physician practice management company, reported a 30% increase in revenue through strategic APP deployment. Similarly, the Cleveland Clinic saw a 15% improvement in patient satisfaction scores following their APP integration initiative. Furthermore, rural health centers, often facing physician shortages, have leveraged APPs to increase patient visits by a remarkable 40-60%, demonstrating the significant impact this strategy can have on access to care.
While the benefits are clear, practices considering APP integration should also be aware of potential challenges. State licensing and scope of practice limitations vary, requiring careful consideration and adherence to local regulations. Supervision requirements and associated liability concerns must also be addressed proactively. Furthermore, reimbursement rates for services provided by APPs are typically lower than those for physicians, which needs to be factored into financial projections. Finally, fostering patient acceptance and trust in APPs is essential for successful integration. Educating patients about the qualifications and expertise of APPs can help build rapport and ensure a smooth transition.
To maximize the benefits of APP integration and increase medical practice revenue, consider these actionable tips:
- Understand state-specific scope of practice laws: Thoroughly research the regulations governing APP practice in your state.
- Develop clear collaborative practice protocols: Establish well-defined guidelines for physician-APP collaboration and communication.
- Invest in APP training and professional development: Support ongoing learning and skill enhancement for your APPs.
- Create efficient billing and coding processes: Ensure accurate and timely billing for APP services to maximize revenue capture.
- Market APP expertise to patients: Highlight the qualifications and capabilities of your APPs to build patient trust and encourage utilization.
Integrating APPs into your medical practice presents a compelling opportunity to increase medical practice revenue, improve patient access, and enhance physician satisfaction. By carefully considering the features, benefits, and potential challenges, and by implementing the tips provided, your practice can successfully leverage the expertise of APPs to achieve sustainable growth and improved patient care. Organizations like the American Association of Nurse Practitioners (AANP) and the American Academy of Physician Assistants (AAPA), as well as successful examples from companies like TeamHealth and Envision Healthcare, offer further resources and insights into best practices for APP integration.
7. Digital Marketing and Online Presence Optimization
In today’s digital age, a robust online presence isn’t just an advantage—it’s a necessity for medical practices looking to thrive. Digital marketing and online presence optimization encompass a range of strategies designed to attract new patients, engage existing ones, and solidify your practice’s reputation within the online landscape. This multifaceted approach leverages various channels and techniques, including search engine optimization (SEO), social media marketing, online reputation management, and targeted advertising, all working in concert to increase patient volume and enhance your practice’s visibility. Failing to prioritize digital marketing can mean missing out on a significant portion of potential patients who actively search for healthcare services online.

Digital marketing works by strategically positioning your practice in front of your target audience at the precise moment they are searching for the services you offer. For example, a well-executed local SEO strategy ensures your practice appears prominently in search results when someone nearby searches for “dermatologist near me.” Social media marketing allows you to engage directly with potential and current patients, building relationships and fostering trust. Online reputation management helps cultivate a positive image of your practice by addressing patient feedback and showcasing testimonials. Finally, paid advertising, like pay-per-click (PPC) campaigns, can quickly amplify your reach and target specific demographics or geographic locations.
The benefits of implementing a comprehensive digital marketing strategy are numerous and often directly impact revenue generation. It offers a cost-effective method of patient acquisition compared to traditional advertising, and its inherent measurability allows you to track your return on investment (ROI) and refine your strategies accordingly. A strong online presence also boosts your practice’s visibility and credibility, establishing you as a trusted authority in your field. Furthermore, it facilitates better patient engagement and fosters loyalty by providing valuable information and convenient communication channels. In a competitive healthcare market, a well-defined digital marketing strategy can give your practice a distinct edge.
Examples of successful digital marketing implementation abound in the healthcare sector. Plastic surgery practices leveraging targeted advertising and social media engagement have reported ROI figures between 200-300%. Dental practices focusing on local SEO often see a 50-100% increase in new patient acquisition. Dermatology practices using social media marketing to showcase before-and-after photos and patient testimonials have documented a 25% growth in patient volume. These examples highlight the powerful impact of digital marketing across various medical specialties.
Despite the numerous advantages, it’s crucial to acknowledge the potential challenges. Digital marketing requires ongoing time and resource investment. The digital landscape is constantly evolving, necessitating continuous learning and adaptation. Navigating healthcare advertising regulations is essential to ensure compliance. Finally, the possibility of negative online reviews and reputation risks requires proactive management.
To effectively implement digital marketing and optimize your online presence, consider these actionable tips:
- Claim and optimize your Google My Business listing: This ensures your practice appears in local search results and provides essential information to potential patients.
- Encourage satisfied patients to leave online reviews: Positive reviews build trust and influence prospective patients.
- Create valuable, educational content for patients: This positions you as an expert and attracts organic traffic to your website.
- Use local SEO strategies to target nearby patients: Optimize your website and content with location-based keywords.
- Monitor and respond to online reviews promptly: Addressing both positive and negative feedback demonstrates attentiveness and professionalism.
Platforms like WebMD, Healthgrades, PatientPop, and BirdEye are widely used by medical practices to manage and enhance their online presence. These platforms offer various tools and services to support digital marketing efforts.
Digital marketing and online presence optimization deserve a prominent place on this list because they are integral to the financial success of modern medical practices. By implementing these strategies effectively, practices can increase patient volume, enhance their reputation, and ultimately, increase medical practice revenue. In a digitally-driven world, embracing these techniques is not just an option; it’s a strategic imperative for sustainable growth and success.
7 Strategies Revenue Growth Comparison
| Strategy | Implementation Complexity 🔄 | Resource Requirements ⚡ | Expected Outcomes 📊 | Ideal Use Cases 💡 | Key Advantages ⭐ |
|---|---|---|---|---|---|
| Revenue Cycle Management (RCM) Optimization | High – technology investment & training | Extensive – automation tools, staff, analytics | Reduced denials, improved cash flow, admin cost savings | Practices needing better financial process control | Reduces claim denials, faster payments |
| Telemedicine and Virtual Care Services | Moderate – platform setup & staff training | Moderate – tech platforms, devices | Expanded patient reach, reduced no-shows, new revenue streams | Practices expanding access and patient convenience | Expands patient base, lowers overhead costs |
| Value-Based Care Contracting | High – data systems & contract complexity | High – analytics, care coordination staff | Higher reimbursements, predictable revenue, better outcomes | Practices focusing on quality and outcome measures | Financial incentives for quality care |
| Ancillary Service Integration | High – capital investment & licensing | High – equipment, specialized staff, space | Multiple revenue streams, higher margins, reduced referrals | Practices wanting in-house comprehensive services | Increased revenue streams per patient |
| Patient Self-Pay and Direct Pay Programs | Moderate – pricing setup & marketing | Moderate – billing system, patient outreach | Higher margins, faster payments, predictable revenue | Practices targeting transparent cash-based care | Reduced admin costs, enhanced doctor-patient relationship |
| Advanced Practice Provider (APP) Integration | Moderate – scope management & supervision | Moderate – APP salaries, training | Increased capacity, reduced physician workload, improved access | Practices expanding care capacity efficiently | Increased patient volume, lower salary costs |
| Digital Marketing and Online Presence Optimization | Moderate – continuous optimization | Moderate – marketing tools, content creation | Increased patient volume, improved visibility and loyalty | Practices aiming to attract and retain patients | Cost-effective acquisition, measurable ROI |
Elevate Your Practice: Implement These Strategies Today
Increasing medical practice revenue in today’s dynamic healthcare environment demands a strategic and comprehensive approach. From optimizing your revenue cycle management (RCM) to embracing digital marketing and expanding service offerings like telemedicine and ancillary services, the strategies discussed in this article provide a roadmap for sustainable growth. Remember that key takeaways like integrating advanced practice providers, exploring value-based care contracts, and offering patient self-pay options can significantly impact your bottom line. Mastering these approaches will not only increase medical practice revenue but also enhance operational efficiency, improve patient satisfaction, and position your practice for long-term success. By embracing innovation and prioritizing patient-centric care, you can navigate the complexities of the healthcare landscape and build a thriving, resilient practice.
Discover how virtual medical receptionists revolutionize healthcare communication—cutting hold times by 100% and boosting patient satisfaction with 24/7 AI-powered scheduling and intake.
Want to further automate routine tasks, optimize patient interactions, and free up staff time to focus on delivering exceptional care? Explore how Simbie AI can help you increase medical practice revenue and streamline your operations. Visit Simbie AI today to learn more.

